Cystatin C: a promising biomarker to evaluate renal function
Cistatina C: um biomarcador promissor para a avaliação da função renal
Janaína Rodrigues Porto1
Karina Braga Gomes2
Ana Paula Fernandes2
Caroline Pereira Domingueti3
1Graduada em Farmácia – Campus Centro Oeste Dona Lindu – Universidade Federal de São João Del Rei – Divinópolis – MG, Brasil.
2Departamento de Análises Clínicas e Toxicológicas, Faculdade de Farmácia, Universidade Federal de Minas Gerais – Belo Horizonte –
MG, Brasil.
3Doutor. Departamento de Análises Clínicas e Toxicológicas, Faculdade de Farmácia, Campus Centro Oeste Dona Lindu – Universidade
Federal de São João Del Rei – Divinópolis – MG, Brasil.
Instituição: Departamento de Análises Clínicas e Toxicológicas, Faculdade de Farmácia, Campus Centro Oeste Dona Lindu – Universidade Federal de São João Del Rei – Divinópolis – MG, Brasil.
Conflito de interesse: sem conflito de interesse.
Artigo recebido em 14/12/2015
Artigo aprovado em 20/04/2016
DOI: 10.21877/2448-3877.201600446
Abstract
Accurate evaluation of the progression of renal function decline is very important, since the early establishment of renoprotective therapies can prevent or delay the occurrence of end stage renal disease. Until now, there is still no ideal biomarker to evaluate glomerular filtration rate, and cystatin C has been demonstrated to be a very promising one. In this review, we have assembled several studies that have evaluated the use of cystatin C to assess glomerular filtration rate in patients with chronic kidney disease, diabetes mellitus and hemodialysis, and also the use of cystatin C to predict the risk of cardiovascular outcomes. Besides cystatin C has been demonstrated by different authors to be equal or superior to the other available renal biomarkers, some limitations still need to be overcome so that cystatin C can be used in clinical to improve the early diagnosis of chronic kidney disease.
Keywords
Cardiovascular diseases; Cystatin C; Diabetic nephropathies; Kidney transplantation; Chronic renal insufficiency
INTRODUction
Chronic kidney disease (CKD) is an important public health problem worldwide, since it is associated with a high morbidity and mortality.(1) It is defined as the presence of abnormalities in renal function for more than three months, with implications to healthy.(2) Patients with renal function impairment show not only a higher risk to develop end stage renal disease, but also to develop cardiovascular events.(1)
Early diagnosis of CKD and the accurate evaluation of the progression of renal function decline and the risk to the development of cardiovascular complications are very important, because the early establishment of reno and cardioprotective therapies can prevent or delay the occurrence of these undesirable outcomes.(2)
Creatinine has been used to evaluate renal function for decades.(3) Different formulas can be used to estimate glomerular filtration rate (GFR) based on creatinine serum levels, such as Cockcroft-Gault, MDRD and CKD-EPI.(4-6) However, all of them have some limitations: Cockcroft-Gault formula tends to overestimate GFR, MDRD formula tends to underestimate it, while CKD-EPI formula has not been extensively studied in different populations yet.(3) As there is still no ideal biomarker to evaluate renal function, new biomarkers have been proposed and cystatin C seems to be a very promising one.(7)
This study aimed to realize a review of the literature about the use of cystatin C to evaluate renal function in different groups of patients, including patients with CKD, diabetes mellitus and hemodialysis, and the utility of cystatin C to predict the risk of cardiovascular outcomes.
Structure and metabolism of cystatin C
Cystatin C has been discovered by Clausen in cerebrospinal fluid in 1961.(8) In the same year, Butler and Flynn(9) detected it in urine. In 1984, Barrett et al.(10) suggested that its physiological function could be the regulation of cystine protease and proposed the name “cystatin C”.
Cystatin C is a non-glycosilated protein with low molecular weight (13kDa), belonging to cysteinoproteases family. It is produced at a constant rate by lysossomes of all nucleated cells in the organism and can be found in several biological fluids, such as serum, seminal liquid and cerebrospinal fluid.(11) Because of its small size and positive charge, cystatin C is freely filtered by renal glomerulus. Unlike creatinine, it is not secreted by renal epithelial tubular cells, although it is reabsorbed. Once it is reabsorbed, it is metabolized by the renal epithelial tubular cells and do not return to bloodstream. Plasma levels of cystatin C seems not to be influenced by muscle mass.(7) However, large doses of glucocorticoids may increase the production of cystatin C and thyroid dysfunction may affect its plasma levels, which is lower in hypothyroidism and higher in hyperthyroidism.(12) In addition, other extra-renal factors, including age, body weight, smoking, C-reactive protein (CRP), cancer, inflammation and steroid therapy may also influence its plasma levels.(13)
Cystatin C and chronic kidney disease
Cystatin C has been shown to be as useful as creatinine to detect GFR reduction in patients with several renal diseases.(7) Some studies have evaluated the use of cystatin C in patients with CKD or with risk to develop CKD are summarized in Table 1. Nitta et al.(14) conducted a study with 140 patients with several renal diseases, aiming to evaluate the clinical application of serum cystatin C as a biomarker of GFR, comparing its levels with clearance of creatinine and clearance of insulin. They observed that serum cystatin C showed a better accuracy than serum creatinine to identify individuals with reduced GFR, indicating that the determination of serum cystatin C is useful to estimate GFR and, particularly, to detect a mild decline of GFR in patients with various renal diseases.
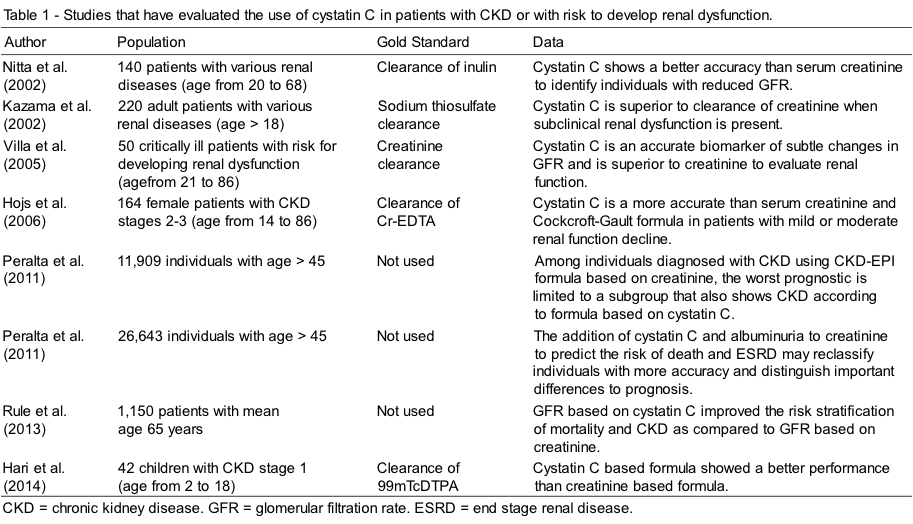
In a similar study, Hojs et al.(15) determined cystatin C and creatinine serum levels and calculated GFR, using Cockcroft-Gault and MDRD formulas, of 164 patients with CKD in stages 2-3 (GFR 30-89mL/min/1.73 m2), whose renal function had been previously evaluated by clearance of Cr-EDTA. They verified that serum cystatin C is a more accurate biomarker of GFR than serum creatinine and than GFR estimated by Cockcroft-Gault formula in female patients with mild or moderate renal function decline.
Kazama et al.(16) evaluated the GFR of 220 patients with various renal diseases by the determination of sodium thiosulfate clearance and compared it with clearance of creatinine, serum creatinine and cystatin C. They concluded that cystatin C is superior to clearance of creatinine when a subclinical renal dysfunction is present. In another study, Villa et al.(17) determined serum creatinine and cystatin C and the clearance of creatinine in 50 critical patients at risk to develop renal dysfunction. They observed that serum cystatin C is an accurate biomarker of subtle changes in GFR and is superior to creatinine to evaluate renal function of these patients.
Peralta et al.(18) conducted a study to compare the classification of CKD by GFR estimated by creatinine and cystatin C. They determined the proportion of patients with GFR < 60 mL/min/1.73 m2, based on creatinine, cystatin C or both, which was estimated by CKD-EPI formulas, in relation to risk of mortality, cardiovascular events and cardiac insufficiency. They evaluated the ability of the GFR estimated by cystatin C to detect additional cases of GFR decline among people with GFR estimated by creatinine ³ 60 mL/min/1.73 m2, and to distinguish a group with a greater risk of chronic renal complications among those with GFR based on creatinine < 60 mL/min/1.73 m2. They observed that among individuals diagnosed with CKD using CKD-EPI formula based on creatinine, the worst prognostic was limited to a subgroup that also had CKD according to the formula based on cystatin C. Therefore, cystatin C may have an important role in the identification of people with CKD that show a higher risk of complications.
In another study, Peralta et al.(19) evaluated whether the combination of creatinine, cystatin C and albuminuria would improve the identification of complications associated with CKD in 26643 patients divided into eight groups defined by GFR based on creatinine < 60 mL/min/1.73 m2, GFR based on cystatin C < 60 mL/min/1.73 m2 and/or albuminuria ³ 30 mg/g, in comparison to creatinine alone. They verified that the association of these three biomarkers improved the discrimination of the risk of death and end stage renal disease. Cystatin C and albuminuria were both strongly and independently associated with death among people with and without CKD defined by GFR based on creatinine. Moreover, the second largest group of risk to end stage renal disease was not detected by creatinine, but it was detected by cystatin C and albuminuria. Therefore, the addition of cystatin C and albuminuria to creatinine to predict the risk may reclassify people with more accuracy and distinguish important differences to prognosis.
Rule et al.(20) evaluated the GFR of 1150 patients with risk factors associated to CKD by the clearance of iothalamate and the formulas based on creatinine, cystatin C or both. They verified that the GFR based on cystatin C improved the risk stratification of mortality and renal insufficiency as compared to GFR based only in creatinine, suggesting that cystatin C may be considered a better biomarker for the risk stratification of CKD. In a study involving 42 children with CKD evaluated by the clearance of 99mTcDTPA, Hari et al.(21) observed that the cystatin C based formula showed a better performance than the formula based on creatinine in children with early CKD.
Cystatin C and diabetes mellitus
Cystatin C has been suggested to provide a better estimative of the GFR than creatinine in diabetic patients.(7) Some studies that have assessed the use of cystatin C to detect renal function decline in diabetic patients are summarized in Table 2. A study conducted by MacIsaac et al.(22) demonstrated that plasma cystatin C was at least as sensible and specific as the GFR estimated by creatinine to detect renal impairment, which was evaluated by isotopic reference, in diabetic patients. Moreover, at normal range of the GFR, the GFR estimated by cystatin C was superior to Cockcroft Gault and MDRD formulas based on creatinine.
In a study involving only type 2 diabetic (DM2) patients, Jeon et al.(23) demonstrated that cystatin C levels increased with increasing of CKD stage from 1 to 3 and from normoalbuminuria to microalbuminuria and showed a positive correlation with albuminuria, indicating that cystatin C is a useful biomarker to detect early renal function decline in DM2 patients, because it reflects both a decrease in the GFR and an increase in albuminuria. It was also verified that cystatin C measurement in urine and serum is a useful biomarker for the evaluation of renal function in DM2 patients with normoalbuminuria.(24)
Pucci et al.(25) analysed the renal function of 288 type 1 (DM1) and DM2 patients by the determination of cystatin C and creatinine plasma levels and the GFR estimated by Cockcroft Gaul and MDRD formulas, and evaluated the efficacy of these biomarkers to detect early renal function decline, comparing to clearance of iohexol. They verified that plasma cystatin C is a better biomarker to early detection of renal function decline than plasma creatinine and the formulas based on creatinine. Similarly, Tan et al.(26) determined the clearance of iohexol in DM1 patients and compared it with plasma creatinine, GFR based on cystatin C, clearance of creatinine and GFR estimated by Cockcroft Gault formula. They observed that cystatin C correlated as well as the clearance of creatinine with the clearance of iohexol, and correlated better than plasma creatinine or the Cockcroft Gault formula.
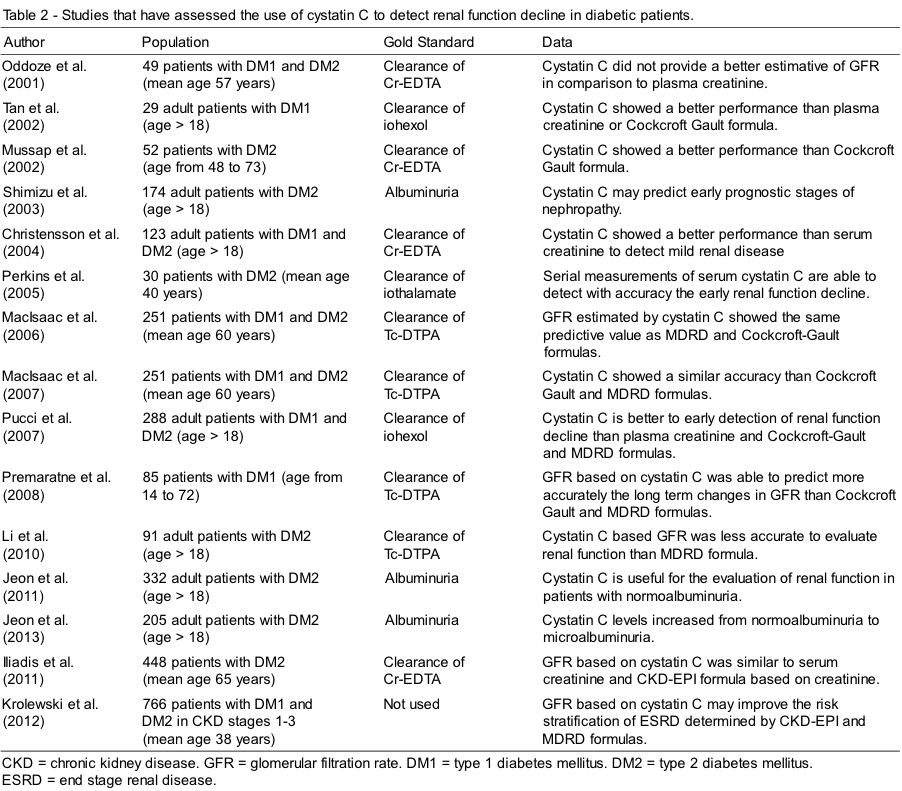
Mussap et al.(27) compared the plasma levels of cystatin C and the GFR estimated by Cockcroft Gault formula, in reference to clearance of 51Cr-EDTA, in DM2 patients to assess which method is more efficient to evaluate the GFR of these patients. They verified that cystatin C showed a better correlation with the clearance of 51Cr-EDTA than the GFR estimated by Cockcroft Gault formula. Furthermore, cystatin C showed a better accuracy to distinguish between patients without renal dysfunction and with renal function decline and provided less false-positive and false-negative results. Shimizu et al.(28) also compared plasma creatinine and cystatin C in 174 DM2 patients and observed that cystatin C is a more sensitive and specific biomarker of the renal function decline than creatinine and may predict early prognostic stages of nephropathy.
Christensson et al.(29) conducted a study with 41 DM1 and 82 DM2 patients in order to determine whether cystatin C is more accurate than serum creatinine to detect diabetic nephropathy. They have reported that serum cystatin C has showed a better performance in comparison to serum creatinine to detect mild renal disease. However, serum creatinine was as efficient as cystatin C to detect severe renal disease. In a study involving 251 diabetic patients, MacIsaac et al.(30) compared the predictive performance of the GFR based on cystatin C with the methods based on creatinine. They reported that the GFR estimated by cystatin C showed the same predictive value as the MDRD and the Cockcroft-Gault formulas. However, they have shown that the adjustment of cystatin C according to clinical and biochemical parameters would improve the predictive value of the GFR based on cystatin C.
Aiming to evaluate the stages of renal disease in diabetes mellitus, Krolewski et al.(31) classified DM1 and DM2 patients in stages 1-3 of CKD, according to the GFR estimated by the CKD-EPI and the MDRD formulas based on creatinine, and by the Stevens formula based on cystatin C. They followed the patients during 10 years to verify whether the prediction of end stage renal disease based on the staging of CKD established by the formulas based on creatinine could be improved by the formula based on cystatin C. Patients classified in a more severe stage of CKD evaluated by the formula based on cystatin C in comparison to the formulas based on creatinine showed a significantly higher risk to develop end stage renal disease, while those classified in a less severe stage of CKD evaluated by the formula based on cystatin C compared to the formulas based on creatinine showed a significantly lower risk. Therefore, the formula based on cystatin C may improve the risk stratification of end stage renal disease determined by the formulas based on creatinine in DM1 and DM2 patients.
Premaratne et al.(32) conducted a study with 85 DM1 patients, who were followed by 10 years, comparing the methods based on creatinine and cystatin C with the clearance of 99mTc-DTPA. They verified that the GFR estimated by cystatin C was more accurate than the GFR estimated by Cockcroft Gault and MDRD formulas based on creatinine to detect renal function decline. Cystatin C was able to predict more accurately the long term changes in GFR when compared to serial determination of GFR calculated by the clearance of 99mTc-DTPA, improving the early identification of patients that show an increased risk to develop kidney failure. Similarly, Perkins et al.(33) assessed the renal function decline in DM2 patients with normal or increased GFR to verify whether cystatin C is able to detect early renal function decline in diabetes mellitus. They have shown that serial measurements of serum cystatin C are able to detect with accuracy the early renal function decline in these patients.
Despite several studies have demonstrated the superiority of cystatin C compared to other renal biomarkers, Oddoze et al.(34) verified that cystatin C did not provide a better estimative of the GFR in comparison to plasma creatinine in 49 patients with diabetes mellitus and renal impairment. Similarly, Li et al.(35) observed that the formulas based on cystatin C provided results less accurate than the MDRD formula based on creatinine to estimate the GFR of 166 patients with CKD and 91 patients with DM2. Iliadis et al.(36) also compared the accuracy of the GFR estimated by formulas based on cystatin C and creatinine in 448 DM2 patients, using the clearance of Cr-EDTA as reference and they verified that the GFR based on cystatin C did not provide a better evaluation of the GFR than the GFR based on creatinine.
Cystatin C and renal transplantation
Cystatin C has been shown to be a more sensitive biomarker to detect early renal dysfunction, which is beneficial to kidney transplant patients, in which small changes of the GFR can impair the post-transplant course.(7) Some studies have evaluated the use of cystatin C to monitor renal function in kidney transplant patients and they are summarized in Table 3. Malheiro et al.(37) compared the predictive performance of the GFR estimated by the MDRD and the Cockcroft Gault formulas based on creatinine with the GFR estimated by the Le Bricon and Stevens formulas based on cystatin C, using as reference the clearance of creatinine, in 173 kidney transplant patients. They observed that the GFR based on cystatin C showed a better efficacy to monitor the graft function than the GFR based on creatinine. In another similar study, Jung et al.(38) analysed 72 kidney transplant patients to compare the clinical efficacy of serum cystatin C and creatinine, in reference to the clearance of creatinine. They reported that cystatin C is a more sensitive biomarker of the reduced GFR (< 60 mL/min/1,73m2) than serum creatinine.
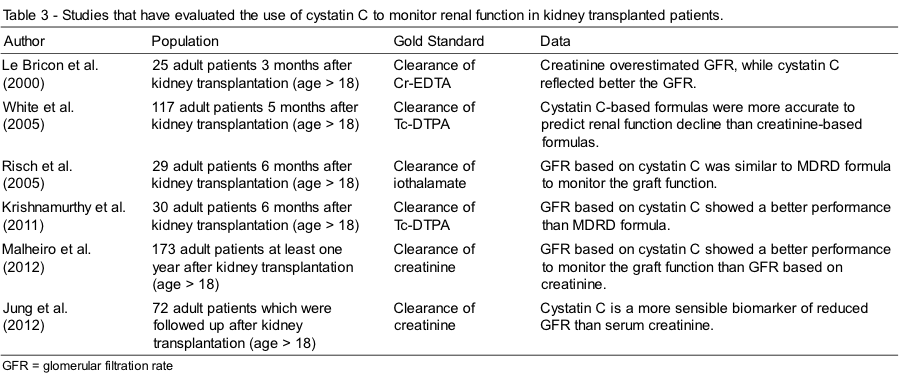
Krishnamurthy et al.(39) compared the efficacy of the GFR estimated by Le Bricon formula based on cystatin C and the GFR estimated by the MDRD formula based on creatinine in 30 patients that have received kidney transplant, using as reference the clearance of Tc-DTPA. They observed that the GFR based on cystatin C showed a better correlation with the clearance of Tc-DTPA than the MDRD formula. White et al.(40) estimated the GFR using four formulas based on cystatin C (Filler, Le Bricon, Larsson and Hoek) and seven formulas based on creatinine, in 117 kidney transplant patients, and compared them with the clearance of Tc-DTPA. They observed that the formulas based on cystatin C were more accurate to predict renal function decline in these patients.
Le Bricon et al.(41) compared plasma cystatin C with the clearance of creatinine and plasma creatinine, three months after the kidney transplant in 25 patients, and verified that creatinine overestimated the GFR, while cystatin C reflected better the GFR and correlated strongly with the clearance of Cr-EDTA. On the other hand, in a study involving 29 kidney transplant patients, Risch et al.(42) verified that the GFR estimated by Larsson formula based on cystatin C was similar to the GFR estimated by MDRD formula based on creatinine to monitor the renal function of these patients.
Cystatin C and cardiovascularrisk
In the last decade, cystatin C has been associated with the risk of cardiovascular disease in elderly population, diabetic patients, individuals with atherosclerosis and patients with CKD, which possibly reflects a very early stage of chronic kidney dysfunction in these individuals.(43-46) Despite cystatin C is not an acute phase protein, it has been shown a significant association between cystatin C and CRP, which is an important biomarker of subclinical chronic inflammation associated with atherosclerosis and CKD.(47) Some studies have assessed the use of cystatin C to predict the risk of cardiovascular disease and they are summarized in Table 4.
Vigil et al.(44) followed 180 patients with CKD diagnosed by the GFR based on creatinine during 6 years. The patients were clustered in tercis according to cystatin C and creatinine values in the beginning of the study. It was analysed whether cystatin C could identify the patients with an increased risk of renal disease progression, death or cardiovascular events. They observed that, unlike creatinine, basal serum cystatin C was a predictor of mortality and of the development of cardiovascular events, suggesting that cystatin C is a usefull biomarker to evaluate cardiovascular morbidity and mortality in patients with CKD.
Schottker et al.(45) evaluated the risk of cardiovascular disease in diabetic patients with CKD, which was defined by the GFR estimated by formulas based on creatinine and cystatin C. They verified that only the definition of CKD based on cystatin C consisted on an independent predictor of the risk of cardiovascular events in diabetic patients, suggesting that the GFR based on cystatin C may show a better clinical utility to predict the cardiovascular risk than the GFR based on creatinine. Shlipak et al.(46) performed a study with 4.637 elderly people in order to compare plasma levels of creatinine and cystatin C as predictors of cardiovascular events and mortality. They showed that the highest levels of cystatin C were directly associated with a higher risk of mortality and that cystatin C was a stronger predictor of cardiovascular events than creatinine and the GFR estimated by creatinine.
In another study, Ix et al.(47) investigated the association between cystatin C with mortality, cardiovascular outcomes and congestive heart failure among 990 individuals with coronary artery disease. They observed that cystatin C serum levels were associated with mortality, cardiovascular outcomes and congestive heart failure. Moreover, high levels of cystatin C were able to predict the increase of the risk of these adverse clinical outcomes, even in individuals without microalbuminuria or reduced GFR. Jernberg et al.(48) also demonstrated that cystatin C improves substantially the risk stratification of the patients with suspected or confirmed non-ST elevation acute coronary syndrome. In other study, Ichimoto et al.(49) reported a prognostic value of cystatin C in patients with myocardial infarction with elevation of ST segment that underwent percutaneous coronary intervention. These authors observed a higher frequency of cardiovascular events among patients with higher plasma levels of cystatin C.
Cepeda et al.(50) have determined the prevalence of higher cystatin C plasma levels in general population, including 415 individuals with more than 49 years old, and its relation with risk factors for cardiovascular disease. They found a high prevalence of individuals with increased levels of cystatin C among those that have cardiovascular risk factors, such diabetes mellitus, CKD and hypertension. They have also observed a correlation between cystatin C levels and biomarkers of cardiovascular risk, such as RPC, homocysteine and fibrinogen. Luc et al.(51) investigated the association between cystatin C plasma levels and the incidence of coronary arterial disease, in a longitudinal study that has involved 9758 healthy men aging between 50 and 59 years old, who were followed during 5 years. They observed that after the adjustment for traditional cardiovascular risk factors (age, diabetes mellitus, tabagism, hypertension, body index mass, triglycerides, cholesterol LDL and HDL), cystatin C was significantly associated with the occurrence of the first ischemic coronary event.
Conclusion
There is still no ideal biomarker to evaluate renal function and cystatin C has been demonstrated to be a very promising one. The studies about the use of cystatin C show divergent results. However, most of them demonstrate that the cystatin C is equal or superior to the other available biomarkers in different groups of patients, such as patients with diabetes mellitus, CKD and kidney transplant. In these patients, cystatin C seems to be especially useful to detect early renal function decline. Moreover, cystatin C has been demonstrated to be an interesting biomarker of cardiovascular risk.
The laboratorial assessment of cystatin C is very expensive and still needs for standardization, and for this reason, it is not widely performed. New studies that confirm the superiority of cystatin C in comparison to methods based on creatinine, or that demonstrate the advantages of the association between these biomarkers to evaluate the GFR of different groups of patients, are still necessary for routinely use of cystatin C in the clinic. The future use of the cystatin C may contribute to improve the early diagnosis of CKD, allowing an early treatment and the prevention of the progression of the CKD and the development of cardiovascular complications.
Acknowlegments
The authors thank FAPEMIG, CAPES and CNPq/Brazil.
Resumo
A avaliação precisa da progressão do declínio da função renal é muito importante, já que o estabelecimento precoce de terapias renoprotetoras pode prevenir ou retardar o desenvolvimento da doença renal terminal. Até o momento, não existe um biomarcador ideal para avaliar a taxa de filtração glomerular, e a cistatina C tem demonstrado ser muito promissora. Nesta revisão, nós reunimos vários estudos que avaliaram o uso da cistatina C para avaliar a taxa de filtração glomerular em pacientes com doença renal crônica, diabetes mellitus e sob hemodiálise, e também o uso da cistatina C para predizer o risco de eventos cardiovasculares. Apesar de ter sido demonstrado por vários autores que a cistatina C é igual ou superior aos outros biomarcadores disponíveis, algumas limitações ainda precisam ser superadas para que a cistatina C possa ser utilizada na clínica para melhorar o diagnóstico precoce da doença renal crônica.
Palavras-chave
Doenças cardiovasculares; Cistatina C; Nefropatias diabéticas; Transplante de rim; Insuficiência renal crônica
REFERENces
- Bastos MG, Bregman R, Kirsztajn GM. Chronic kidney diseases: common and harmful, but also preventable and treatable. Rev Assoc Med Bras. 2010;56:248-53.
- Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl. 2013; 3:1-150.
- Cirillo M. Evaluation of glomerular filtration rate and of albuminuria/proteinuria. J Nephrol. 2010;23:125-32.
- Cockcroft DW, Gault MH. Prediction of creatinine clearance from serum creatinine. Nephron. 1976;16:31-41.
- Levey AS, Greene T, Kusek JW, Beck GJ, GROUP MS. A simplified equation to predict glomerular filtration rate from serum creatinine [Abstract]. J Am Soc Nephrol. 2000;11:A0828.
- Levey AS, Stevens LA, Schmid CH, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150:604-12.
- Massey D. Commentary: clinical diagnostic use of cystatin C. J Clin Lab Anal. 2004;18:55-60.
- Clausen J. Protein in normal cerebrospinal fluid not found in serum. Proc Soc Biol Med.1961;107:170-2.
- Butler EA, Flynn FV. The occurrence of part-gamma protein in urine: a new protein abnormality. J Clin Pathol. 1961;14:172-8.
- Barret AJ, Davies ME, Grubb A. The place of human gamma trace (cystatin C) amongst the cysteine proteinase inhibitors. Biochem Biophys Res Commun. 1984;120:631-6.
- Murussi M, Murussi N, Campagnolo N, Silveiro AP. Early detection of diabetic nephropathy. Arq Bras Endrocrilon Metab. 2008; 53:442-51.
- Filler G, Bokenkamp A, Hofmann W, Le Bricon T, Martínez-Brú C, Grubb A. Cystatin C as a marker of GFR-history, indications, and future research. Clin Biochem. 2005;38:1-8.
- Macissac RJ, Premaratne E, Jerums G. Estimating glomerular filtration rate in diabetes using serum cystatin C. Clin Biochem Rev. 2011;32: 61-7.
- Nitta K, Hayashi T, Uchida K, et al. Serum cystatin C concentration as a marker of glomerular filtration rate in patients with various renal diseases. Intern Med. 2002;41:931-5.
- Hojs R, Bevc S, Ekart R, Gorenjak M, Puklavec L. Serum cystatin C as an endogenous marker of renal function in patients with mild to moderate impairment of kidney function. Nephrol Dial Transplant. 2006;21:1855-62.
- Kazama JJ, Kutsuwada K, Ataka K, Maruyama H, Gejyo F. Serum cyastatin C reliably detects renal dysfunction in patients with various renal diseases. Nephron. 2002;91:13-20.
- Villa P, Jiménez M, Soriano MC, Manzanares J, Casasnovas P. Serum cystatin C concentrations as a marker of acute renal dysfunction in critically ill patients. Crit Care. 2005;9:139-43.
- Peralta CA, Katz R, Sarnak MJ, et al. Cystatin C identifies chronic kidney disease patients at higher risk for complications. J Am Soc Nephrol. 2011;22:147-55.
- Peralta CA, Shlipak MG, Judd S, et al. Detection of chronic kidney disease with creatinine, cystatin C, and urine albumin-to-creatinine ratio and association with progression to end-stage renal disease and mortality. JAMA. 2011;305:1545-52.
- Rule AD, Bailey KR, Lieske JC, Peyser PA, Turner ST. Estimating the glomerular filtration rate from serum creatinine is better than from cystatin C for evaluating risk factors associated with chronic kidney disease. Kidney Int. 2013;83:1169-76.
- Hari P, Ramakrishnan L, Gupta R, Kumar R, Bagga A. Cystatin C-based glomerular filtration rate estimating equations in early chronic kidney disease. Indian Pediatr. 2014;51:273-7.
- MacIsaac RJ, Tsalamandris C, Thomas MC, et al. The accuracy of cystatin C and commonly used creatinine based methods for detecting moderate and mild chronic kidney disease in diabetes. Diabet Med. 2007;24:443-8.
- Jeon YL, Kim MH, Lee WI, Kang SY. Cystatin C as an early marker of diabetic nephropathy in patients with type 2 diabetes. Clin Lab. 2013;59:1221-9.
- Jeon YK, Kim MR, Huh JE, et al. Cystatin C as an early biomarker of nephropathy in patients with type 2 diabetes. J Korean Med Sci. 2011;26:258-63.
- Pucci L, Triscorna S, Lucchesi D, et al. Cystatin C and estimatives of renal function: searching a better measure of kidney function in diabetic patients. Clin Chem. 2007;53:480-8.
- Tan GD, Lewis AV, James TJ, Altmann P, Taylor RP, Levy JC. Clinical usefulness of cystatin C for the estimation of glomerular filtration rate in type 1 diabetes: reproducibility and accuracy compared with standard measures and iohexol clearance. Diabetes Care. 2002; 25:2004-9.
- Mussap M, Dalla Vestra M, Fioretto P, et al. Cystatin C is a more sensitive marker than creatinine for the estimation of GFR in type 2 diabetic patients. Kidney Int. 2002;61:1453-61.
- Shimizu A, Horikoshi S, Rinno H, Kobata M, Saito K, Tomino A. Serum cystatin C may predict the early prognostic stages of patients with type 2 diabetic nephropathy. J Clin Lab Anal. 2003;17:164-7.
- Christensson AG, Grubb AO, Nilsson JA, Norrgren K, Sterner G, Sundkvist G. Serum cystatin C advantageous compared with serum creatinine in the detection of mild but not severe diabetic nephropathy. J Intern Med. 2004;256:510-8.
- MacIsaac RJ, Tsalamandris C, Thomas MC, et al. Estimating glomerular filtration rate in diabetes: a comparision of cystatin C and creatinine-based methods. Diabetologia. 2006;49:1686-9.
- Krolewski AS, Warram JH, Forsblom C, et al. Serum concentration of cystatin C and risk of end-stage renal disease in diabetes. Diabetes Care. 2012;35:2311-6.
- Premaratine E, MacIsaac RJ, Finch S, Panagiotopoulos S, Ekinci E, Jerums G. Serial measurements of cystatin C are more accurate than creatinine-based methods in detecting declining renal function in type 1 diabetes. Diabetes care. 2008;31:971-3.
- Perkins BA, Nelson RG, Ostrander BE, et al. Detection of renal function patients with diabetes and normal or elevated GFR by serial measurements of serum cystatin C concentration: results of a 4-year follow-up study. J Am Soc Nephrol. 2005;6:1404-12.
- Oddoze C, Morange S, Portugal H, Berland Y, Dussol B. Cystatin C is not more sensitive than creatinine for detecting early renal impairment in patients with diabetes. Am J Kidney Dis. 2001;38: 310-6.
- Li HX, Xu GB, Wang XJ, Zhang XC, Yang JM. Diagnostic accuracy of various glomerular filtration rates estimating equations in patients with chronic kidney disease and diabetes. Chin Med J. 2010;123:745-51.
- Iliadis F, Didangelos T, Ntemka A, et al. Glomerular filtration rate estimation in patients with type 2 diabetes: creatinine-or cystatin C based equations? Diabetologia. 2011;54:2987-94.
- Malheiro J, Fonseca I, Martins LS, et al. A comparison between serum creatinine and cystatin C based equations for estimation of graft function. Transplant Proc. 2012;44:2352-6.
- Jung YJ, Lee HR, Kwon OJ. Comparison of serum cystatin C and creatinine as a marker for early detection of decreasing glomerular filtration rate in renal transplants. J Korean Surg Soc. 2012;83:69-74.
- Krishnamurtthy N, Arumugasamy K, Anand U, Anand CV, Aruna V, Venu G. Serum cystatin C levels in renal transplant recipients. Indian J Clin Biochem. 2011;26:120-4.
- White C, Akbari A, Hussain N, Dinh L, Lepage N, Knoll GA. Estimating glomerular filtration rate in kidney transplantation: a comparison between serum creatinine and cystatin C-based methods. J Am Soc Nephrol. 2005;6:3763-70.
- Le Bricon T, Thervet E, Froissart M, et al. Plasma cystatin C is superior to 24 h creatinine clearance and plasma creatinine for estimation of glomerular filtration rate 3 months after kidney transplantation. Clin Chem. 2000;46:1206-7.
- Risch L, Huber AR. Assessing glomerular filtration rate in renal transplant recipients by estimates derived from serum measurements of creatinine and cystatin C. Clin Chim Acta. 2005;356:204-11.
- Vigil A, Condés E, Vigil L, et al. Cystatin C as a predictor of mortality and cardiovascular events in a population with chronic kidney disease. Int J Nephrol. 2014;2014:127943.
- Schöttker B, Herder C, Müller H, Brenner H, Rothenbacher D. Clinical utility of creatinine and cystatin C based definition of renal function for risk prediction of primary cardiovascular events in patients with diabetes. Diabetes Care. 2012;35:879-86.
- Shlipak MG, Sarnak MJ, Katz R, et al. Cystatin C and the risk of death and cardiovascular among elderly persons. N Engl J Med. 2005;352:2049-60.
- Ix JH, Shlipak MG, Chertow GM, Whooley MA. Association of cystatin C with mortality, cardiovascular events, and incident heart failure among persons with coronary heart disease: data from the Heart and Soul Study. Circulation. 2007;115:173-9.
- Bökenkamp A, Herget-Rosenthal S, Bökenkamp R. Cystatin C, kidney function and cardiovascular disease. Pediatr Nephrol. 2006; 21(9):1223-30.
- Jernberg T, Lindahl B, James S, Larsson A, Hansson LO, Wallentin L. Cystatin C: a novel predictor of outcome in suspected or confirmed non-ST-elevation acute coronary syndrome. Circulation. 2004;110 (16):2342-8.
- Ichimoto E, Jo K, Kobayashi Y, Inoue T, Nakamura Y, Kuroda N, et al. Prognostic significance of cystatin C in patients with ST-elevation myocardial infarction. Circ J. 2009;73(9):1669-73.
- Cepeda J, Tranche-Iparraguirre S, Marín-Iranzo R, et al. Cystatin C and cardiovascular risk in the general population. Rev Esp Cardiol. 2010;63(4):415-22. [Article in Spanish].
- Luc G, Bard JM, Lesueur C, Arveiler D, Evans A, Amouyel P, et al. Plasma cystatin C and development of coronary heart disease: The PRIME Study. Atherosclerosis. 2006;185(2):375-80.
Correspondência
Caroline Pereira Domingueti
Rua Sebastião Gonçalves Coelho, 400 – Chanadour
35501-296 – Divinópolis – MG, Brasil
