Biochemical parameters of crack users in different therapies
Parâmetros bioquímicos de usuários de crack em diferentes terapias
Denilson R. Fonseca1, Louyse Sulzbach Damázio2, Mathias de Brida1, Adalberto Alves de Castro1, Lara Canever1, Daniela V. Bavaresco1, Alexandra Ioppi Zugno1
1 UNESC, Programa de Pós-Graduação em Ciências da Saúde – Criciúma, SC, Brasil.
2 UNESC, Nutrição; Programa de Pós-Graduação em Ciências da Saúde – Criciúma, SC, Brasil.
Recebido em 18/02/2022
Aprovado em 02/12/2022
DOI: 10.21877/2448-3877.202200022
INTRODUCTION
In Brazil, as well as many other countries, drug misuse in general, and also crack addiction, in particular, are expanding in an alarming rate.(1,2) All over the world, substance use disorder remains a condition of difficult approach, with a very high rate of unsuccessful treatment and severe implications on the whole society.(3)
In this context, studying the outcomes of harm reduction and abstinence approach is of great value, for improving both methods in the future. The socio-demographic profile of crack users in Brazil comprises mostly young adults with an average age of 30 years, unemployed, with low education and income, from dysfunctional families. Usually, the patient who is addicted to crack has a history of multiple substances use disorder.(4,5) The most conventional treatment for drug users in abstinence is usually in a psychiatric sector of a hospital, including all the standard medical and psychosocial support, both public and private health systems can hardly provide access for all the population in need.(2)
The Federal Government has given priority to outpatient care and reduced the number of hospital beds in psychiatric sectors all over the country, both for financial and ideological reasons.(6) Outpatient care is represented in the public health system, by the Centers of Psychosocial Care (CAPS). CAPS are defined as daycare outpatient services and are divided into care modalities, among them the CAPS ad is intended for the care of patients with disorders resulting from the use and dependence of psychoactive substances.(7) The government has permitted the existence of Non-Governmental organizations that offer “inpatient” care an alternative treatment based on total isolation of the outside world in a clinic, where there is little or, more frequently, no conventional medical/psychosocial care and thus, no medication is administered to the patients.(8) These places are called Therapeutic Communities (CT).
Research correlating neurobiological factors, chemical dependence, and changes in that remain scarce, thus, opening a new investigation field. It is known that psychiatric disorders are also associated with the levels of neurotrophins, a family of proteins that regulate several aspects of neuronal development and functions, including the formation of synapses and synaptic plasticity. The main neurotrophins, among mammals, are neuronal growth factor (NGF) and brain-derived neurotrophic factor (BDNF). The present study aimed to compare two methods of treating drug misuse: Total Abstinence, offered at a CT versus Harm Reduction, offered at CAPS.(9)
MATERIAL AND METHODS
This is an observational case-control study. Patients were allowed to quit the research at any time, without any loss in their treatment process or the privacy of their data. The project was approved by the Ethics Committee of the Universidade do Extremo Sul Catarinense (UNESC) by protocol number 208.255-28/02/2013. The groups were: CAPS and CT (Baseline, 7 days, and 3 months). To the biochemical analyzes were added the group of healthy controls from the blood collection laboratory and matched by age and gender.
The subjects of the present research were selected according to proper inclusion criteria, in two places for treatment of substance addiction in the city of Criciúma, State of Santa Catarina, Brazil. The CAPS for Alcohol and Other Drugs (CAPS-ad) was one of the places, and the other a CT.
The sample of the study was selected according to the following criteria: age 18 years or over, being in treatment in one of the institutions named above, minimum of 5 years of schooling (thus, illiteracy was a criterion of exclusion), score Alcohol, Smoking, and Substance Involvement Screening Test (ASSIST) (measuring drug use) equal or superior to 16, voluntarily accepting participating the study, and having the use of crack as the most used substance (in quantity and frequency); but the use of other substances was not an exclusion criterion.
During 18 months, the patients of the present study were selected and subjected to tests. The present study included 49 patients, being 21 in the CAPS and 28 CT group, and 16 healthy controls. The invitations were done in person by the researchers in the institutions. The individuals who fit the inclusion criteria and signed the Informed Consent were evaluated for substance misuse by applying the ASSIST (Alcohol, Smoking and Substance Involvement Screening Test) score, and the patients who reached 16 points or more were classified as possibly drug-dependent, and eligible for the study. After the inclusion, the following evaluations were proposed to the patients:
- Evaluation of psychiatric conditions by the Structured Clinical Interview for DSM Disorders (SCID-I).(10)
- ASSIST. A structured questionnaire containing eight questions on nine classes of psychoactive substances (tobacco, alcohol, marijuana, cocaine, and others). The questions address the frequency of use in life and the last three months, problems related to use, concern about the use by people close to the user, loss of performance of expected tasks, unsuccessful attempts to cease or reduce use, feeling of compulsion and use by injection. Each response corresponds to a score, from 0 to 4, and the total sum can vary from 0 to 20. The score range from 0 to 3 is considered as indicative of occasional use, from 4 to 15 as indicative of abuse and >16 as suggestive of dependence.(11)
- Biochemical analysis: Blood samples were collected after 3 months of treatment, to detect long term alterations of the treatments (but not short-term effects due to drug abstinence syndrome). At the end of the interviews and psychological testing, blood was collected and was centrifuged at the Laboratory of Translational Psychiatry (UNESC). Then, we performed the analysis of plasma levels of Brain-Derived Neurotrophic Factor (BDNF), Nerve Growth Factor (NGF) and Neuron Specific Enolase (NSE), this was done analysis using kits commercially available for immunoenzymatic methods (ELISA – enzyme-linked immunosorbent assay, Bioscience, San Diego, CA, USA).
For biochemical analyzes, the CAPS and CT groups stand out, had another subdivision, had better results demonstrated, and, therefore, deepened as discussions about the respect of the findings of this study. Thus, forming the crack group (CAPS plus CT) and the control group, without differentiating as treatment methods in the first stage of this assessment.
RESULTS
In this work, a total sample was 49 men, of these 21 from CAPS and 28 from CT. The mean age was 35 years, while the CAPS group had an average of 41.5 years or the CT group was 26 years old (difference p <0.001). The average time of crack use was 12 years, in the CAPS group or the average time was 17 years and in the CT group 10.5 years, with no statistically significant difference (p=0,14). The results of the Scoreno ASSIST for cocaine remained with an average of 29 in the general sample, without the CAPS 29 group and the CT 25.5 group (p=0,32). The average value of the two groups and isolated from them exceeded 16, indicating dependence.
Results for SCID-I scores are summarized in Table 1. The present work showed no significant differences between CAPS and CT groups in time of crack abstinence, alcohol use, other addictions, current depression, Bipolar Disorder, current suicidal ideation, and past suicidal ideation. The present work found, however, that CAPS patients had significantly higher scores (compared to CT group) of psychosis (p=0,02*) and previous history of depression (p=0,03*).
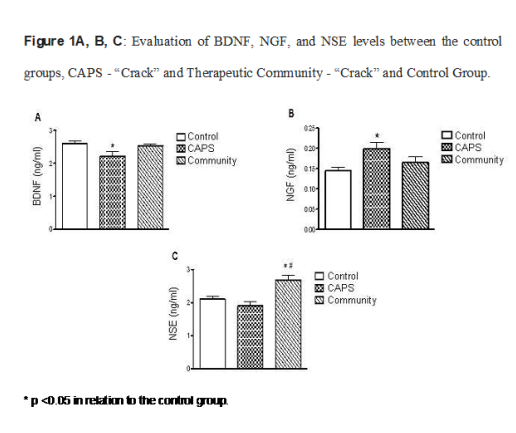
Figure 1 A, B, C
Evaluation of BDNF, NGF, and NSE levels between the control groups, CAPS – “Crack” and Therapeutic Community – “Crack” and Control Group.
* p <0.05 in relation to the control group.
Table 1
Distribution of results regarding the qualitative variables of dependence and comorbidity according to SCID-I, presented in both institutions and the total sample.
|
|
CAPS
(n=21) |
Therapeutic Community (n=28) |
Total
(n=49) |
Chi-Square Test | |
| Abstinence Time | Up to 7 days | 9 (43%) | 16 (57%) | 25 (51%) | χ² = 0,98 |
| Abstinence | 3 Months or + | 12 (57%) | 12 (43%) | 24 (49%) | p=0,32 |
| Alcohol Dependency | Absence | 6 (29%) | 14 (50%) | 20 (41%) | χ² = 2,28 |
| Present | 15 (71%) | 14 (50%) | 29 (59%) | p=0,13 | |
| Other dependece | Absence | 0 (0%) | 2 (7%) | 2 (4%) | χ² = 1,56 |
| Present | 21 (100%) | 26 (93%) | 47 (96%) | p=0,50 | |
| Current Depression | Absence | 11 (52%) | 21 (75%) | 32 (65%) | χ² = 2,71 |
| Present | 10 (48%) | 7 (25%) | 17 (35%) | p=0,10 | |
| Past Depression | Absence | 4 (19%) | 14 (50%) | 18 (37%) | χ² = 4,95 |
| Present | 17 (81%) | 14 (50%) | 31 (63%) | p=0,03* | |
| Dysthymia | Absence | 15 (71%) | 24 (86%) | 39 (80%) | χ² = 0,22 |
| Present | 6 (29%) | 4 (14%) | 10 (20%) | p=0,29 | |
| Bipolar Disorder | Absence | 17 (81%) | 25 (89%) | 41 (86%) | χ² = 0,41 |
| Present | 4 (19%) | 3 (11%) | 7 (14%) | p=0,44 | |
| Psychosis | Absence | 3 (14%) | 13 (46%) | 16 (33%) | χ² = 5,64 |
| Present | 18 (86%) | 15 (54%) | 33 (67%) | P=0,02* | |
| Current | Absence | 14 (67%) | 20 (71%) | 34 (69%) | χ² = 1,23 |
| Suicide Ideation | Present | 7 (33%) | 8 (29%) | 15 (31%) | p=0,72 |
| Suicidal | Absence | 8 (38%) | 15 (54%) | 23 (47%) | χ² = 1,15 |
| Past Ideation | Present | 13 (62%) | 13 (46%) | 26 (53%) | p=0,28 |
χ² test and Chi-square; * statistical difference of p <0.05.
DISCUSSION
CAPS patients had significantly higher scores of previous depression and psychosis. One important difference was in the age, being CAPS patients significantly older than their CT counterparts. Such differences, being CAPS patients older and previously more affected by psychiatric conditions, possibly induced long term alterations in their bodily and neuronal metabolisms, which may no longer be reversed by any treatment currently available.(12)
Cognitive deficit is related to alterations of neurotrophic factors level such as brain-derived neurotrophic factor (BDNF), nerve growth factor (NGF). In this sense, we evaluate these neurotrophins in subjects and our results showed that BDNF levels were increased in CAPS group compared with the CT group. BDNF is a peptide whose role is pivotal in neurogenesis and cell survival. It is altered in conditions related to psychological trauma,(13) major depression disorder,(14) and bipolar disorder.(15) Lower BDNF levels among CAPS patients are likely to have been influenced by previous conditions like a history of depression, and current higher psychosis scores as well.(16)
However, as the amount of occasional use of alcohol, drugs, and even adhesion to prescribed medications was not monitored, it is impossible to infer which of these factors may have influenced over the lower BDNF levels verified among CAPS patients.
NGF levels were increased among CAPS patients. One plausible hypothesis is alcohol occasional use,(17) which was present among CAPS patients and was impossible among CT patients, because of the inherent isolation and hard control of this method of treatment. Another possible cause of the increased NGF levels is the use of certain antidepressants.(18)
Our work has serious limitations, mostly the absence of a control group of healthy individuals psychiatric evaluations, and the absence of women in our sample. However, the treatment of CT in complete isolation lacking any prescribed or illicit drugs have some of the characteristics of a “positive control” group.
An overview of our results suggests that most of them reflect, actually, the previous conditions of our patients, rather than the kind of social or professional treatment received. Interestingly, low BDNF levels, as found in the CAPS group, are also a feature of depressed patients(19), and patients of CAPS group had higher “past depression” scores than CT patients. Differences in BDNF, and NGF between CAPS and CT results may have happened due to older age and higher severity of psychiatric conditions among CAPS patients. Increased NSE levels among CT patients support the hypothesis that total drug abstinence without medical support is a risk factor for increased NSE levels.
CONCLUSION
Considering the problematic field of drugs of abuse, with an emphasis on crack, it was concluded that a methodological proposal of treatment, regardless of its approach, needs to offer care with a biopsychosocial approach and in the perspective of integrality. In conclusion, both methods may have benefits and harms according to the patients’ profile, which must be addressed in futures studies.
FUNDING SOURCES
Universidade do Extremo Sul Catarinense.
ACKOWLEDGEMENTS
The university, the CAPS and the entire team get involved in the study.
REFERENCES
- Obot IS, Poznyak V, Monteiro M. From basic research to public health policy: WHO report on the neuroscience of substance dependence. Addict Behav. 2004; 29(7): 1497-502.
- Ferreira Filho OF, Turchi MD, Laranjeira R, Castelo A. Epidemiological profile of cocaine users on treatment in psychiatrics hospitals. Rev Saúde Pública. 2003; 37(6):751-9.
- Whiteford HA, Ferrari AJ, Degenhardt L, Feigin V, Vos T. Global burden of mental, neurological and substance use disorders: an analysis from the Global Burden of Disease Study. In: Patel V, Chisholm D, Dua T, Laxminarayan R, Medina-Mora ME. Mental, Neurological, and Substance Use Disorders: Disease Control Priorities, PloS One. 2015;10:e0116820.
- Cruz M, Bertoni N, Bastos FI, Burnett C, Gooch J, Fischer B. Comparing key characteristics of young adult crack users in and out-of-treatment in Rio de Janeiro, Brazil. Subst Abuse Treat Prev Policy. 2014; 10; 9:2.
- Nappo SA, Galduróz JC, Raymundo M, Carlini EA. Changes in cocaine use as viewed by key informants: a qualitative study carried out in 1994 and 1999 in São Paulo, Brazil. J Psychoactive Drugs. 2001; 33(3): 241-53.
- Domanico A, Malta M. Implementation of harm reduction toward crack users in Brazil: barriers and achievements. Subst Use Misuse. 2012; 47(5): 535-46.
- BRASIL. Portaria nº 336, de 19 de fevereiro de 2002. Dispõe sobre a proteção e os direitos das pessoas portadoras de transtornos mentais e redireciona o modelo assistencial em saúde mental. Brasília. 2002.
- Van der Meer Sanchez Z, Nappo SA. Religious treatments for drug addiction: an exploratory study in Brazil. Soc Sci Med. 2008; 67(4):638-46.
- Stone KA. Reviewing harm reduction for people who inject drugs in Asia: the necessity for growth. Harm Reduct J. 2015; 12:32.
- Sanchez-Villegas A, Schlatter J, Ortuno F, Lahortiga F, Pla J, Benito S et al. Validity of a self-reported diagnosis of depression among participants in a cohort study using the Structured Clinical Interview for DSM-IV (SCID-I). BMC Psychiatry. 2008; 8:43.
- WHO ASSIST Working Group. The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): Development, reliability, and feasibility. Addiction. 2002; 97(9):1183–94.
- Kontis D, Huddy V, Reeder C, Landau S, Wykes T. Effects of age and cognitive reserve on cognitive remediation therapy outcome in patients with schizophrenia. Am J Geriatr Psychiatry. 2013; 21(3):218-30.
- Angelucci F, Ricci V, Gelfo F, Martinotti G, Brunetti M, Sepede G et al. BDNF serum levels in subjects developing or not post-traumatic stress disorder after trauma exposure. Brain Cogn. 2014; 84(1):118-22.
- Fiorentini A, Volonteri LS, Dragogna F, Rovera C, Maffini M, Mauri MC et al. Substance-induced psychoses: a critical review of the literature. Curr Drug Abuse Rev. 2011; 4(4):228-40.
- Tunca Z, Ozerdem A, Ceylan D, Yalçin Y, Can G, Resmi H et al. Alterations in BDNF (brain derived neurotrophic factor) and GDNF (glial cell line-derived neurotrophic factor) serum levels in bipolar disorder: The role of lithium. J Affect Disord. 2014;166:193-200.
- Tan YL, Zhou DF, Cao LY, Zou YZ, Zhang XY. Decreased BDNF in serum of patients with chronic schizophrenia on long-term treatment with antipsychotics. Neurosci Lett. 2005; 382(1-2):27-32.
- Kleine TO, Benes L, Zöfel P. Studies of the brain specificity of S100B and neuron-specific enolase (NSE) in blood serum of acute care patients. Brain Res Bull. 2003; 61(3):265-79.
- Engel D, Zomkowski AD, Lieberknecht V, Rodrigues AL, Gabilan NH. Chronic administration of duloxetine and mirtazapine downregulates proapoptotic proteins and upregulates neurotrophin gene expression in the hippocampus and cerebral cortex of mice. J Psychiatr Res. 2013; 47(6):802-8.
- Bus BA, Molendijk ML, Tendolkar I, Penninx BW, Prickaerts J, Elzinga BM et al. Chronic depression is associated with a pronounced decrease in serum brain-derived neurotrophic factor over time. Mol Psychiatry. 2015; 20(5):602-8.
Correspondência
Louyse Sulzbach Damázio
E-mail: [email protected]
