Characterization of the Transgender Male Population in Rio Grande do Norte and Its Relationship with the Pap Smear
Received on 07/01/2024
Approved on 07/18/2024
DOI: 10.21877/2448-3877.202400190.en
INTRODUCTION
Transsexuality is a complex phenomenon that transcends medical and biological definitions, encompassing cultural and social dimensions. Transgender individuals are those who, within cultural contexts, experience a dissonance with the gender assigned at birth and seek to modify it in various ways—not exclusively through surgical or hormonal interventions. This diverse and multifaceted experience involves issues of identity, authenticity, and self-determination, with varied expressions of gender.(1)
Historically, transsexuality has long been associated with bodily modifications. During the second half of the twentieth century, there was exponential growth in health technologies, especially those aimed at body modification. Initially developed for soldiers returning mutilated from wars, these technologies also inspired masculinized lesbian women—known as butches—and trans men. This development proved important for trans men’s engagement with new body-modification technologies, allowing them to shape their bodies and perform the gender identities they sought.(2)
The transgender population frequently encounters significant barriers to accessing healthcare, primarily due to stigma and discrimination from healthcare professionals, as well as the lack of specialized services and the high financial costs associated with gender transition. Furthermore, the absence of specialized training among professionals—resulting from a cultural denial of the existence of trans people—may lead to critical gaps in the provision of adequate care and the failure to recognize the specific needs of the trans population.(3)
It is essential to recognize the gender identity of trans men and to respect their self-determination. These are individuals assigned female at birth who identify within the male gender spectrum. The use of testosterone and surgical procedures, such as chest reconstruction, are some of the ways in which trans men affirm their gender identity.(4)
In the context of cervical cancer, trans men who have not undergone hysterectomy remain at risk and require screening exams. However, a lack of awareness and preparedness among healthcare professionals—combined with the discomfort and anxiety experienced by these patients during the procedure—results in low adherence to screening. It is therefore crucial that healthcare services be prepared to address the specific needs of trans men, ensuring equal access to care.(5)
Cervical cancer is a complex and multifaceted condition, with persistent infection by Human Papillomavirus (HPV) as its main predisposing factor. HPV is a virus commonly transmitted through sexual contact, and its presence in the body can lead to the development of precancerous lesions and cervical cancer. Infection typically occurs through microlesions in the epithelium of the ectocervix, the outer portion of the cervix facing the vaginal canal. The virus has the capacity to invade the basal epithelial cells—particularly at the squamocolumnar junction, where the two types of cervical epithelium (simple columnar and stratified squamous) meet—where it replicates and releases its genetic material (DNA). This viral replication process may trigger an abnormal cellular response, leading to excessive and disorganized proliferation of epithelial cells.(6)
According to the 2023 Annual Report by the Brazilian National Cancer Institute José Alencar Gomes da Silva (INCA),(7) excluding non-melanoma skin tumors, cervical cancer is the third most incident type of cancer among cisgender women in Brazil. For each year within the 2023–2025 triennium, an estimated 17,010 new cases are expected. In the North and Northeast regions, it ranks as the second most common cancer. Specifically for the state of Rio Grande do Norte, 280 new cases are projected during this period. In 2021, according to the same report, the cervical cancer mortality rate in Brazil was 4.51 deaths per 100,000 women, while in the Northeast region it was higher, at 5.61 deaths per 100,000 cisgender women.
It is important to note that all data related to cervical cancer published by the INCA(7) refer exclusively to cisgender women and not to individuals with a cervix. As such, trans men were excluded from these statistics, which can be attributed to the lack of health programs targeted at this population and their low adherence to screening, resulting from the various barriers previously mentioned. This leads to the underreporting of cervical cancer cases among trans men. Notably, no official data on this topic exist for the state of Rio Grande do Norte. Given the scarcity of such records, the present study aims to characterize the clinical and laboratory profiles of trans men treated in Rio Grande do Norte, with a focus on Pap smear screening and statistical analysis of the collected data.
MATERIALS AND METHODS
This is a cohort study based on a quantitative and qualitative analysis of medical records of trans men treated over the past four years at the Instituto de Medicina Tropical – IMT Clínico do Rio Grande do Norte, specifically at the Trans and Travesti Outpatient Clinic of Natal (known as TT Outpatient Clinic – “Ambulatório TT”– and affiliated with Giselda Trigueiro Hospital – HGT), which provides multidisciplinary care exclusively through Brazil’s Unified Health System (Sistema Único de Saúde – SUS).
The patients’ medical records and cervical cancer screening histories were reviewed. Each record was assessed for the following variables: (1) age; (2) occupation; (3) marital status; (4) residence; (5) place of birth; (6) sexual orientation; (7) hormone therapy use; (8) history of sexually transmitted infections (STIs); (9) history of mastectomy; (10) regularity of Pap smear screening; and (11) result of the most recent exam.
It is important to emphasize that no identifying patient information was used or disclosed in this study. The activity was authorized by the HGT Permanent Education Unit (Appendix 1), and access to the documentation was granted in accordance with Brazilian National Health Council Resolution No. 510/2016, specifically Article 1, Sole Paragraph, Item V.(8)
This resolution addresses the ethical guidelines for research involving data obtained directly from participants or from identifiable information that may pose risks beyond those encountered in everyday life. According to the sole paragraph, Item V, the CEP/CONEP system will neither register nor evaluate “V – research using databases with aggregated information, with no possibility of individual identification.”
The collected data were analyzed using IBM SPSS Statistics® version 20.0.
RESULTS AND DISCUSSION
A total of 80 medical records were analyzed, covering the period from February 2020 to March 2024. These records represent all transgender men followed by the multidisciplinary team at the TT Outpatient Clinic during this period in the state of Rio Grande do Norte. The age of the patients ranged from 9 to 55 years, with the majority (62.5%) between 20 and 29 years old (Figure 1). There is no established explanation in the specialized literature for the higher prevalence of this age group among patients seen at the TT Outpatient Clinic in Natal. However, based on information from the medical records, it is hypothesized that this predominance may be related to individuals from these generations being more concerned about their health or seeking body modifications through hormone therapy. Nevertheless, further research is required to substantiate and confirm this assumption.
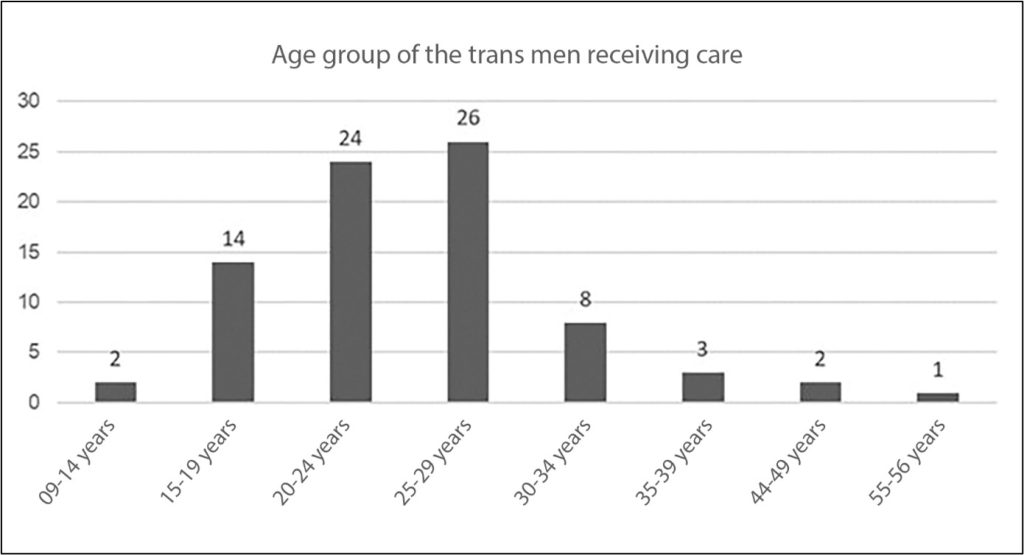
Figure 1
Age group of trans men receiving care.
Note: Interruptions in the sequence of age groups are due to the absence of patients in the 40–43, 50–54, and 57 years or older categories during the analyzed period; therefore, these data were not included in the table.
A cross-analysis of data on patients’ age and occupation revealed that the most frequent occupational categories were students (31.2%) and unemployed individuals (12.5%) (Table 1). Five individuals chose not to disclose their occupation, and 29 reported various other roles, including lawyer, public servant, kitchen assistant, general services assistant, bartender, barbecue chef, fast-food worker, supermarket employee, private driver, teacher, telemarketer, security guard, and salesperson, among others. It was also reported that most transgender men receiving care resided in the capital city, Natal (53.75%), followed by Parnamirim (22.5%), totaling 17 municipalities across the state (Table 2).
The fact that most transgender men in this study were either students or unemployed may be associated with the deeply rooted prejudice in Brazilian society, which hinders the inclusion of these individuals in the labor market. This statement is supported by multiple data sources. In Brazil, for instance, the number of murders of trans individuals increased by more than 10% in 2023 compared to 2022. Notably, while the country continued to be the largest consumer of trans pornography on adult content platforms, it also remained, for the fifteenth consecutive year, the nation with the highest number of trans people murdered globally.
The Northeast region ranks second in the country in terms of trans homicides, accounting for approximately 36% of cases recorded between 2017 and 2023, just behind the Southeast region with 37%. These figures are compounded by the persistent underreporting of anti-LGBTQIA+ violence.(8) These realities expose the multiple challenges faced by the transgender population—not only in seeking dignified employment, but also in defending their fundamental right to life.
Regarding hormone therapy, it was found that the majority of participants were undergoing treatment, representing approximately 73.7% (Table 3), which aligns with findings in the literature. In this context, hormone use has become the first and most significant body modification technology employed by trans men seeking gender-affirming changes—often considered even more essential than genital reassignment surgery.(1) However, this practice can be risky, as many participants reported having initiated hormone therapy independently, without medical supervision. The hormone used by trans men in this therapy is testosterone, and although its distribution is regulated by law, unsupervised hormone use continues to occur. This exposes individuals to health risks, as such treatment plans are often fragile or inadequate due to the absence of specialized healthcare supervision.(2)
Table 1
Occupation by age group
| Occupation by age group | Not reported | Unemployed | Self-employed | Barber | Elementary and High School Student | University Student | Other |
| 9-14 years | 0 | 0 | 0 | 0 | 2 | 0 | 0 |
| 15-19 years | 1 | 0 | 1 | 0 | 9 | 3 | 0 |
| 20-24 years | 0 | 3 | 2 | 2 | 0 | 7 | 10 |
| 25-29 years | 2 | 4 | 1 | 2 | 0 | 4 | 13 |
| 30-34 years | 1 | 3 | 1 | 1 | 0 | 0 | 2 |
| 35-39 years | 1 | 0 | 0 | 1 | 0 | 0 | 1 |
| 44-49 years | 0 | 0 | 0 | 0 | 0 | 0 | 2 |
| 55-56 years | 0 | 0 | 0 | 0 | 0 | 0 | 1 |
| Total: 80
(100%) |
5
(6.2%) |
10
(12.5%) |
5
(6.2%) |
6
(7.5%) |
11
(13.8%) |
14
(17.5%) |
29
(36.3%) |
Note: Interruptions in the sequence of age groups are due to the absence of patients in the 40–43, 50–54, and 57+ age groups during the analyzed period; for this reason, these data were not included in the table.
Table 2
Place of Residence of Trans Men Receiving Care at the TT Outpatient Clinic.
| Residence | Number |
| Natal | 43 |
| Parnamirim | 18 |
| Caicó | 2 |
| Ceará Mirim | 2 |
| João Câmara | 1 |
| Jucurutu | 1 |
| Macaíba | 1 |
| Nova Cruz | 1 |
| Parelhas | 1 |
| São Gonçalo | 3 |
| São José do Mipibu | 1 |
| Santana dos Matos | 1 |
| São Rafael | 1 |
| Santa Cruz | 1 |
| Lajes | 1 |
| Guamaré | 1 |
| Doutor Severiano | 1 |
Table 3
Age Group × Use of Hormone Therapy
| Age group | Not Reported | Undergoing Therapy | Not Undergoing Therapy |
| 9-14 years | 1 | 0 | 1 |
| 15-19 years | 0 | 6 | 8 |
| 20-24 years | 0 | 19 | 5 |
| 25-29 years | 0 | 23 | 3 |
| 30-34 years | 0 | 6 | 2 |
| 35-39 years | 0 | 2 | 1 |
| 44-49 years | 0 | 2 | 0 |
| 55-56 years | 0 | 1 | 0 |
| Total: 80
(100%) |
1
(1.3%) |
59
(73.7%) |
20
(25%) |
Note: Interruptions in the sequence of age groups are due to the absence of patients in the 40–43, 50–54, and 57+ age groups during the analyzed period. For this reason, these data were not included in the table.
Regarding marital status, during the multidisciplinary care provided at the outpatient clinic, 32 individuals reported being single, 32 in a relationship, 13 were married, and three chose not to disclose this information. The most prevalent sexual orientation was heterosexual (58.75%), followed by bisexual (12.5%), pansexual (2.5%), and homosexual (1.25%). Twenty individuals chose not to report their sexual orientation (Table 4).
Sexual orientation and gender identity are distinct aspects of the human experience. When a trans man (an individual assigned female at birth who identifies and lives as a man) is attracted to women, he is heterosexual; if he is attracted to men, he is homosexual. Accordingly, trans men—like any other group—may have various sexual orientations: heterosexual, homosexual, bisexual, pansexual, asexual, among others.(9)
According to the 2023 Annual Report from INCA, in 2019,(7) 81.3% of cisgender women in the target age group across Brazil had undergone a Pap smear less than three years prior to the interview date. However, the Northeast region reported the lowest rate among all regions, with approximately 76.4% of cisgender women up to date with their screening.
Table 4
Marital Status by Sexual Orientation
| Marital status by sexual orientation | Not Reported | Heterosexual | Bisexual | Homosexual | Pansexual |
| Not Reported | 3 | 0 | 0 | 0 | 0 |
| Single | 5 | 17 | 8 | 1 | 1 |
| Married | 3 | 9 | 1 | 0 | 0 |
| In a relationship | 9 | 21 | 1 | 0 | 1 |
| Total: 80
(100%) |
20
(25%) |
47
(58.8%) |
10
(12.5%) |
1
(1.2%) |
2
(2.5%) |
Table 5
Regular Pap Smear Screening by Age Group
| Age group | Not Reported | Does Not Undergo | Undergoes |
| 9 a 14 | 1 | 1 | 0 |
| 15 a 19 | 0 | 13 | 1 |
| 20 a 24 | 0 | 21 | 3 |
| 25 a 29* | 0 | 18 | 8 |
| 30 a 34* | 0 | 6 | 2 |
| 35 a 39* | 0 | 2 | 1 |
| 44 a 49* | 0 | 2 | 0 |
| 55 a 56* | 0 | 0 | 1 |
| Total | 1 | 63 | 16 |
* Age group prioritized for Pap smear screening (25 to 64 years) according to the Cervical Cancer Screening Guidelines – INCA.(9)
Note: Interruptions in the sequence of age groups reflect the absence of patients in the 40–43, 50–54, and 57+ age groups during the study period. For this reason, these data were not included in the table.
In the present study, 40 trans men fell within the age group recommended as a priority for cervical cancer screening. Of these, only 12 (30%) reported undergoing the Pap smear regularly. In other words, 70% of the trans men treated at the outpatient clinic, who should undergo routine cytological screening for cervical cancer, were not doing so (Table 5). These figures may be linked to the prejudice this population faces within healthcare settings. These findings are alarming, as these men remain vulnerable to the disease and require preventive monitoring through regular screening.
All transgender men whose medical records were analyzed in this study had not undergone hysterectomy, retaining both uterus and vagina. Therefore, like cisgender women, they are subject to diseases associated with these organs, such as cervical cancer.(5) Thus, cervical cancer screening is necessary for this population.
According to the Cervical Cancer Screening Guidelines –INCA,(10) in Brazil, the cytopathological exam should be prioritized for women aged 25 and older who have been sexually active. The exam should be performed annually, and if two consecutive annual results are negative, it may be performed every three years thereafter. Screening should continue until age 64 and may be discontinued if, after that age, there are at least two negative results within the previous five years. Although the guidelines refer exclusively to cisgender women, thereby excluding trans men, they should be equally applied to this population, which also requires regular screening. Trans men are often at increased risk due to higher exposure to HPV, resulting from various social vulnerabilities.
When analyzing regular Pap smear screening rates by occupation among trans men at the time of care, low adherence was found across all categories: 80% of the unemployed, 100% of the self-employed, 83.3% of barbers, and 78.6% of university students reported not undergoing regular cervical cancer screening (Table 6). It would be expected that students would have higher screening rates than other occupational groups, as access to education and healthcare tends to be directly proportional—greater access to education generally correlates with increased attention to disease prevention and health maintenance.(11)
Although the results aligned with expectations, the overall rate remained very low. When compared to data on cisgender women, only 21.4% of transgender men who were university students reported undergoing the Pap smear regularly. However, according to the 2019 National Health Survey by IBGE (Brazilian Institute of Geography and Statistics),(12) 72.5% of cisgender women with incomplete elementary education had undergone the exam within the previous three years, while 90.4% of those with a completed university degree did so regularly.
Regarding marital status, it was observed that only 15.3% of married trans men underwent the preventive exam regularly, whereas the screening rates were higher among single individuals (18.7%) and those in a relationship (25%) during the period in which they were seen (Table 7). This may be linked to the false belief that having a steady partner reduces the risk of contracting sexually transmitted infections such as HPV and, consequently, the likelihood of developing cervical cancer.(13)
Considering only the two municipalities with the highest prevalence of patients treated at the TT Outpatient Clinic (Natal and Parnamirim), only 18.6% of trans men residing in Natal were up to date with cervical cancer screening. In contrast, among those residing in the municipality of Parnamirim, 22.2% had undergone the exam within the last three years.
Regarding sexual orientation, 76.6% of heterosexual participants reported not undergoing the exam; none of the bisexual or pansexual individuals did, while all homosexual participants stated that they did. These findings are also linked to whether or not the individual had engaged in penetrative sex, as HPV is most often transmitted through sexual contact via microlesions in the epithelium caused by penetration.
As a result, many healthcare professionals may not consider the Pap smear a priority for those who have never engaged in penetrative sex, whether penis–vagina or any object inserted into the vaginal canal.(14) However, for those who have experienced penetration, regular cervical screening through the Pap smear is necessary. In this study, among those who had engaged in penetrative sex, 69.2% did not undergo the Pap smear regularly, and only 30.8% did (Figure 2). These findings are considered alarming, as these individuals are at risk of developing cervical cancer.
Table 6
Regular Pap Smear Screening by Occupation
| Not Reported | Unemployed | Self-employed | Barber | Elementary and High School Student | University Student | Other | |
| Not Reported | 0 | 0 | 0 | 0 | 1 | 0 | 0 |
| Does Not Undergo | 3 | 8 | 5 | 5 | 10 | 11 | 21 |
| Undergoes | 2 | 2 | 0 | 1 | 0 | 3 | 8 |
| Total: 80
(100%) |
5
(6.2%) |
10
(12.5%) |
5
(6.2%) |
6
(7.5%) |
11
(13.8%) |
14
(17.5%) |
29
(36.3%) |
Table 7
Regular Pap Smear Screening by Marital Status
| Marital Status | Not Reported | Single | Married | In a relationship | Total | |
| Regular Pap Smear Screening | Not Reported | 1 | 0 | 0 | 0 | 1 |
| Does Not Undergo | 2 | 26 | 11 | 24 | 63 | |
| Undergoes | 0 | 6 | 2 | 8 | 16 | |
| 3
(3.7%) |
32
(40%) |
13
(16.3%) |
32
(40%) |
80
(100%) |
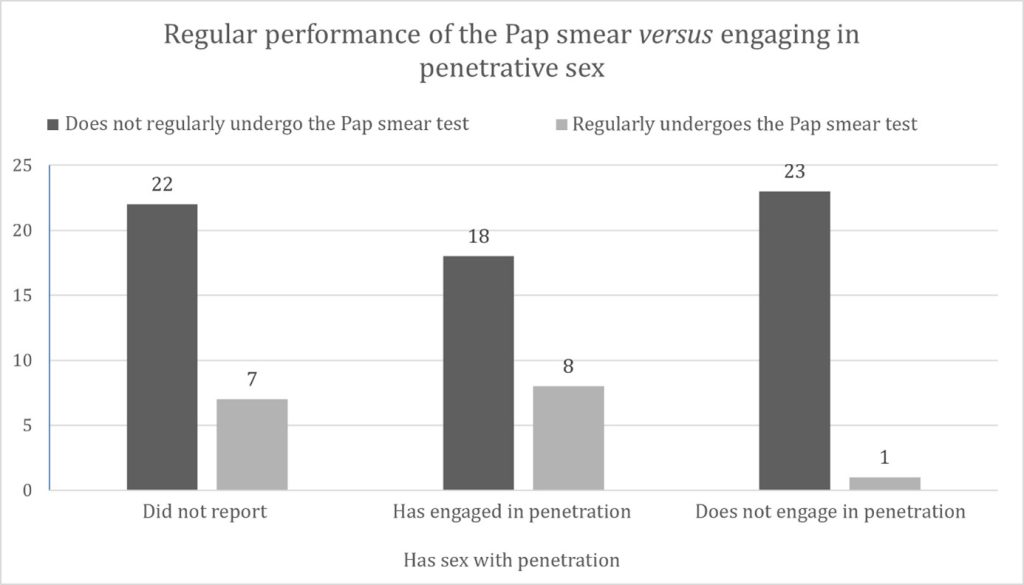
Figure 2
Regular Pap Smear Screening versus History of Penetrative Sexual Activity
Of the 80 trans men whose medical records were analyzed, only 16 (20%) regularly underwent the Pap smear. Among them, 9 (56.3%) did not report the result of their most recent exam, and 7 (43.7%) had a negative result for intraepithelial lesion or malignancy (NILM) (Figure 3).
In this context, Technical Note No. 1/2024-INCA/DIDEPRE/INCA/CONPREV/INCA/SAES/MS(15) was recently issued, providing guidance to SUS administrators regarding changes in cervical cancer screening methods in Brazil. It includes molecular biology techniques for HPV detection and self-collection—yet it is directed exclusively toward cisgender women and girls, thereby excluding the transgender male population.
Accordingly, this study and all the data presented here align with the limited body of literature on this topic in Brazil, demonstrating that the vast majority of transgender men are neither included in healthcare services nor in public policies for cervical cancer screening. As a result, they remain largely invisible and, consequently, marginalized.
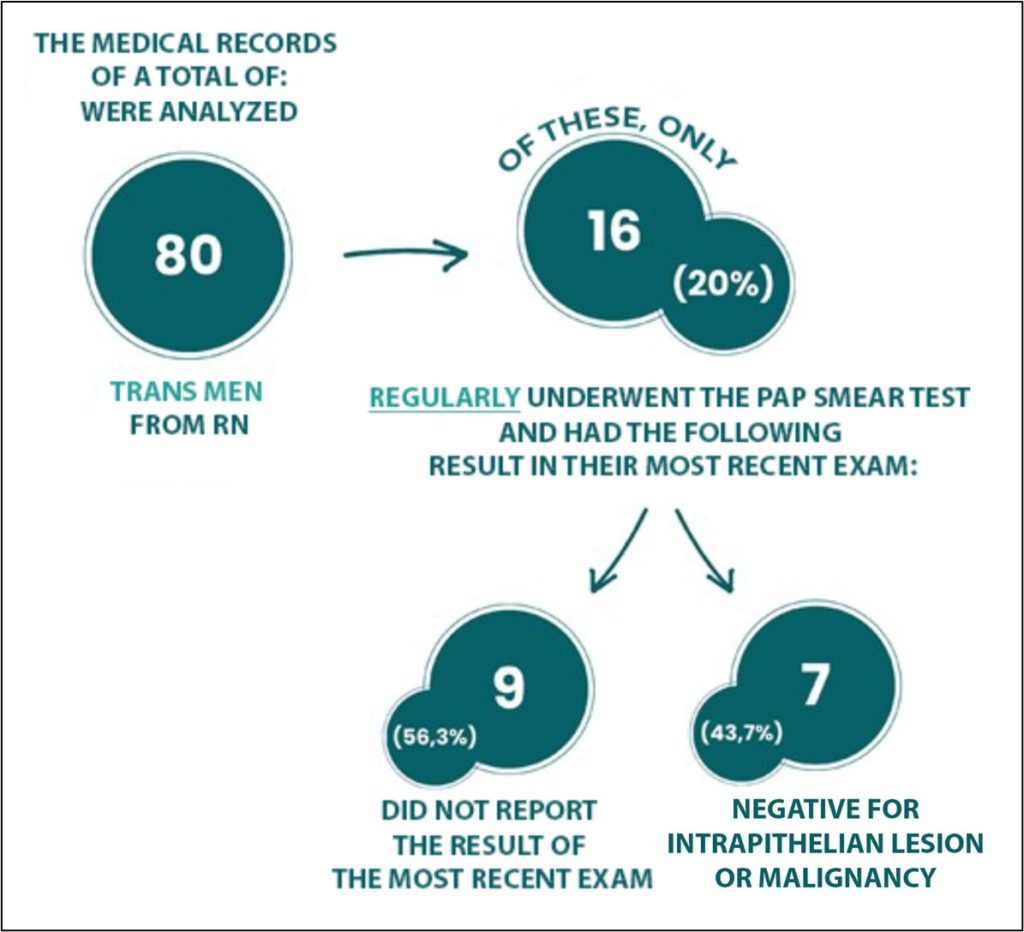
Figure 3
NILM Result
FINAL CONSIDERATIONS
This scenario underscores the urgent need for changes in public health. It is essential to include trans men through the development of specific guidelines based on scientific research and lived trans experiences, while also promoting new studies, investments, and the dissemination of clinics—such as the TT Outpatient Clinic—that provide inclusive care and guidance for regular Pap smear screening.
Training healthcare professionals is another crucial step in improving care for the transgender population. It is vital that students, during their academic education, are exposed to this subject and trained to provide respectful, affirming care—acknowledging chosen names and avoiding stigmatizing behavior.
The Pap smear must be recognized as an inclusive exam for all individuals with a cervix, not exclusively for women. This change should begin with targeted communication campaigns and extend to the adaptation of services through the creation of neutral and inclusive clinics—breaking the association between the Pap smear and performative femininity.
ACKNOWLEDGMENTS
We would like to thank the entire team of the TT Outpatient Clinic, Giselda Trigueiro Hospital, and the Instituto de Medicina Tropical – IMT Clínico of Rio Grande do Norte for providing the materials necessary for the development of this study. We also express our sincere gratitude and respect to all the transgender men of Rio Grande do Norte who contributed their data for the epidemiological understanding of this population.
REFERENCES
- Ribeiro CR, Ahmad AF, Dantas BS, Lemos A. Masculinidades em construção, corpos em (re)construção: desejos, contradições e ambiguidades de homens trans no processo transexualizador. Cien Saúde Colet. outubro de 2022;27(10):3901–11.
- Sousa D, Iriart J. “living with dignity’’’: Health needs and demands of trans men in Salvador, Bahia State, Brazil”. Cad Saúde Pública. 2018;34(10).
- Dias JPB, Pietrafesa GAB, Silva SA da. Acesso e utilização da atenção ginecológica na atenção primária à saúde: percepção do homem transexual. Saúde e Pesquisa. 28 de novembro de 2023;16(4):1-15.
- Stark B, Hughto JMW, Charlton BM, Deutsch MB, Potter J, Reisner SL. The contraceptive and reproductive history and planning goals of trans-masculine adults: a mixed-methods study. Contraception. 1o de dezembro de 2019;100(6):468-73.
- Arruda PM, Oliveira MGL, Colares IA, Britto DF, Peixoto RAC. Saúde sexual e reprodutiva de homens transgêneros e mulheres homoafetivas: Revisão Integrativa. Research, Society and Development. 27 de janeiro de 2022;11(2):e35311225676.
- da Silva RCG, Silva AC de O, Peres AL, de Oliveira SR. Profile of women with cervical cancer attended for treatment in oncology center. Revista Brasileira de Saúde Materno Infantil. 1o de outubro de 2018;18(4):695–702.
- INSTITUTO NACIONAL DE CÂNCER (Brasil). Dados e números sobre câncer do colo do útero: relatório anual 2023. Rio de Janeiro: INCA, 2023. Available at: https://www.inca.gov.br/publicacoes/relatorios/dados-e-numeros-sobre-cancer-do-colo-do-utero-2023. Accessed on: June 6, 2024.
- BENEVIDES, B. G. Dossiê: assassinatos e violências contra travestis e transexuais brasileiras em 2023. São Paulo: ANTRA, 2024. Available at: https://antra.org.br/dossie-antra-2023/. Accessed on: June 6, 2024.
- RODRIGUEZ, A. Experiências de atenção à saúde e percepções das pessoas transgênero, transexuais e travestis sobre os serviços públicos de saúde em Florianópolis/SC, 2013–2014. 2014. 132 f. Dissertação (Mestrado em Saúde Coletiva) – Universidade Federal de Santa Catarina, Florianópolis, 2014. Available at: https://repositorio.ufsc.br/handle/123456789/128486. Accessed on: June 6, 2024.
- Instituto Nacional de Câncer (Brazil). Diretrizes brasileiras para o rastreamento do câncer do colo do útero. 2011. 101 p.
- Arteaga Rodríguez C, Kolling MG, Mesquida P. Educação e Saúde: um Binômio que Merece Ser Resgatado. Health and Education: a Binomial worth being rescued. Vol. 31. 2007.
- IBGE Diretoria de Pesquisas, Coordenação de Trabalho e Rendimento. Pesquisa Nacional de Saúde 2019. 2019.
- Araújo JM da S, Santos MMG, Silva RS da, Martins M de CV, Gallotti FCM. Exame de Papanicolaou e câncer cervical em homens transgêneros: revisão integrativa. Research, Society and Development. 9 de fevereiro de 2021;10(2):e17010212342.
- Agénor M, Peitzmeier SM, Bernstein IM, Mcdowell M, Alizaga NM, Reisner SL, et al. Perceptions of cervical cancer risk and screening among transmasculine individuals: patient and provider perspectives. Vol. 18, Source: Culture, Health & Sexuality. 2016.
- Ministério da Saúde (BR), Secretaria de Atenção Especializada à Saúde, Instituto Nacional de Câncer, Coordenação de Prevenção e Vigilância, Divisão de Detecção Precoce e Apoio à Organização de Redes. NOTA TÉCNICA Nº 1/2024-INCA/DIDEPRE/INCA/CONPREV/INCA/SAES/MS. Brasília: Ministério da Saúde; 2024. 2p.
Correspondence
Breno Figueiredo Souza
E-mail: [email protected]
