Detection of carbapenem hydrolyzing enzyme and extended spectrum beta-lactamase in clinical isolates of Enterobacteriaceae and Pseudomonaceae
Detecção de enzimas hidrolizantes de carbapenemas e beta-lactamases de espectro estendido em isolados clínicos de Enterobacteriaceae e Pseudomonaceae
Gabriel de Oliveira Santos1
Renato Silva Teixeira2
1Graduando em Ciências Biológicas. Associação Educacional Dom Bosco. Resende-RJ, Brasil.
2Doutor. Professor em Associação Educacional Dom Bosco. Resende-RJ, Brasil.
Instituição: Associação Educacional Dom Bosco. Resende-RJ, Brasil.
Recebido em 25/10/2019
Aprovado em 11/09/2020
DOI: 10.21877/2448-3877.202100919
INTRODUCTION
The emergency of strains of enterobacterias resistant to the carbapenem has become a public health problem due to our limited therapeutical arsenal available to treat infections caused by multiresistant micro-organisms, in Brasília, Brazil, public and private hospitals report the presence of Carbapenemase producing strains since 2010.(1) The resistance to antibiotics has increased in the last few years in Brazil and the world, creating an increasing necessity for knowledge of the resistance profile and the way this resistance is disseminated by the bacteria that most frequently cause infections.(2)
From 524 isolates in hospitals in Brasilia, Brazil, between 2011 and 2013, 74% of the strains are Klebsiella pneumoniae (388 strains), these isolates showed high frequency of resistance to the b-lactams tested where de minor frequency detected was 88% to Imipenem.(1) The ESBL constitute an enzyme group derivated of the classicals Beta-lactamases, these enzymes granted the bacteria resistance to the broad-spectrum cephalosporin, penicillins and monobactams (Aztreonam), but they remain sensitive to the Cephamycins and Carbapenems.(2)
During a study realized in 1998 through 1999 were identified 38 of 44 patients with infections caused by E. coli and K. pneumoniae ESBL producing but only 33 had open medical records.(3) From this 33, 25 patients had infections caused by Klebsiella and 8 by Escherichia, and the sites of infection were: genitourinary tract in 17 patients; wounds in 5 patients; intravenous catheter in 4 patients; blood in 3 patients; respiratory tract in 3 and “abdomen” in one. This alert us to the fact that these species that live with us in an ecological relation of protocooperation could cause infections in several tissue and systems and the possibility that this organisms could be producing ESBL or any kind of carbapenemase aggravate even more the infections that depend exclusively of the patient’s immune system, something that we can’t control, and our contact with them is daily given that their habitat could be the water, soil and our own skin.
When facing this resistant micro-organisms, the effective way to fight them is using more and more dangerous drugs such as Polymyxin B and Tigecycline, administrated intravenous, they have a series of restrictions and require a close monitoring of the renal function and liver function despite the fact that they cause irreversible damage such as bone discoloration and weakness of dentition.
Material and methods
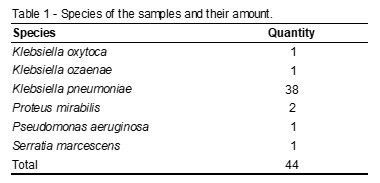
All the samples were acquired through donation from various patients from Rio de Janeiro hospitals. Most of them were from oral swab, rectal swab, oropharynx swab and unique swab from neonatal patients during September, 2018 through July, 2019. The number of isolates and their respective species are shown at Table 1.
The samples were frozen at a temperature of -20°C in 2 mL of Brain Hearth Infusion broth (BHI) with 25% glycerin until the moment of the tests. The tests were conducted as recommend by the Clinical Laboratory Standards Institute (CLSI),(4) in virtue to realize the ESBL test the samples were reactivated in 2 mL BHI broth at 37°C for 24 hours and then strewed in Agar Mueller Hinton and returned to the incubator at 37°C for 18 hours. After the growth was prepared the inoculums with the colonies at 0,5 McFarland in 0,9% sterile saline solution, right after the inoculums were strewed at Agar Mueller Hinton and placed an Amoxicillin with clavulanic acid at the center and four discs at 20 mm of distance from it, the used drugs were: aztreonam, cefotaxime, ceftazidime and ceftriaxone. The positive result of this test is given by the appearance of a “ghost zone” between the discs.
For the modified Hodge test was used the ATCC EC25922 and the ATCC KP1705 strains for the positive control of the tests. First, it was strewed the ATCC EC25922 strain at the Mueller Hinton Agar and then placed an Imipenem disc at the center. After that, with an inoculating needle, it’s strewed the ATCC KP1705 for positive control in a line from the disc to the extremity of the dish, the same is applied to the strain to be tested. For this test the positive result is given by a distortion at the inhibition zone cause by the enzymes produced by the tested strain that allows the sensitive ATCC EC25922 strain to grow.
Results
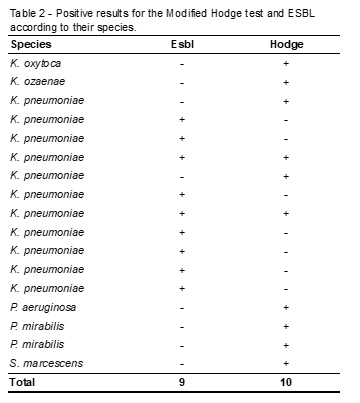
From the 44 samples analyzed nine were strains that produced ESBL and ten strains produced some kind of Carbapenemaseas shown below (Table 2).
Discussion
The isolation of this multidrug-resistant strains demonstrates that their occurrence is even more frequently than it was a few years ago, in 2011 from 345 isolates only 4% were KPC producing.(5) It confirms that the number of this strains has increased since the first one was identified in 2001.(6) The two samples that produced both ESBL and KPC are the actual main concern to doctors and health professionals because if, somehow, they get to cause an infection, its treatment will be through intravenous antibiotics that cause neurotoxicity, nephrotoxicity, liver toxicity and also could be teratogenic such as the Tigecycline. Their number continue to increase what makes them a public health issue even thou it has not the epidemiologic character they are a serious problem for those hospitalized or immune suppressed. Most of the isolates received came from patients in ICUs what confirms that theses bacterias affect mostly those who are immunosuppressed. Based on this data it’s clear the necessity of decrease the use of antibiotics whenever it’s possible, realizing its proper disposure and also sets an alert to our hygiene habits given the fact that we most likely have more than one species of an Enterobacteria colonizing our digestor tract so with poor hygiene habits the self-inflicted infection could happen and it also could contaminate areas of common use of the family or population.
Resumo
Objetivo: Caracterizar isolados de enterobactérias e pseudomonas em relação a sua resistência aos antimicrobianos. Métodos: O estudo foi realizado com 44 amostras de várias espécies das famílias Enterobacteriaceae e Pseudomonaceae, as quais foram submetidas aos testes de Hodge Modificado e Beta-Lactamase de Espectro Estendido (ESBL). Resultados: Das 44 amostras analisadas nove são produtoras de ESBL e dez são produtoras de carbapenemase. Conclusão: No total, 38,6% das amostras apresentaram algum tipo de resistência às ESBL e carbapenemases, e esse número mostra um aumento na incidência dessas resistências nos últimos anos já que, antes de 2001, não haviam sido descritas as enzimas carbapenemases. Esse fato é alarmante para pacientes imunossuprimidos ou hospitalizados uma vez que as enterobactérias colonizam nosso trato digestivo e podem causar uma infecção se dada a oportunidade.
Palavras-chave
Resistência beta-lactâmica; Enterobacteriaceae; Pseudomonas
REFERÊNCIAS
- Faria Junior C. Caracterização de cepas de Enterobacteriaceae resistentes a carbapenens isoladas no Distrito Federal. 2014. 87 f., il. Master’s Thesis – Universidade de Brasília, Brasília, 2014.
- Tosin I, Silbert S, Sader HS. The use of molecular typing to evaluate the dissemination of antimicrobial resistance among gram-negative rods in Brazilian hospitals. Braz J Infect Dis [online]. 2003, vol.7, n.6 [cited 2019-08-26], pp.360-369. Available from: <http://www. scielo. br/scielo.php?script=sci_arttext&pid=S1413-86702003000600002&lng=en&nrm=iso>.ISSN1413-8670. http://dx.doi.org/10.1590/S1413-86702003000600002.
- Lautenbach E, Patel JB, Bilker WB, Edelstein PH, Fishman NO. Extended-Spectrum b-Lactamase-Producing Escherichia coli and Klebsiella pneumoniae: Risk Factors for Infection and Impact of Resistance on Outcomes, Clinical Infectious Diseases, Volume 32, Issue 8, 15 April 2001, Pages 1162-1171, <https://doi.org/10.1086/319757>.
- Clinical and Laboratory Standards Institute. 2016. Performance standards for antimicrobial susceptibility testing; 26 ed. CLSI supplement M100S. Clinical and Laboratory Standards Institute, Wayne, PA.
- Ribeiro, VB. Detecção de resistência aos carbapenêmicos e avaliação da produção de Klebsiella pneumoniae Carbapenemase (KPC) em isolados da família Enterobacteriaceae. 2013. Doctor’s Thesis – Universidade Federal do Rio Grande do Sul, 2013.
- Yigit H, Queenan AM, Anderson GJ, Domenech-Sanchez A, Biddle JW, Steward CD, et al. Novel carbapenem-hydrolyzing beta-lactamase, KPC-1, from a carbapenem-resistant strain of Klebsiella pneumoniae. Antimicrobial agents and chemotherapy vol. 45,4 (2001): 1151-61. doi:10.1128/AAC.45.4.1151-1161.2001.
Correspondência
Renato Silva Teixeira
Av. Cel Prof. Antonio Esteves, nº 01 – Campo de Aviação
27.523-000 – Resende-RJ, Brasil
