Giant Cell Arteritis – A Case Report
Arterite de Células Gigantes – Um Relato de Caso
Paulo Moacir Mesquita-Filho1, Luciano Bambini Manzato1, Daniel Lima Varela1, Rubens Rodrigues2, Wagner Lazaretto Padua3, Laura de Cezaro Martini4, Artur Eduardo Martio4, Taís Otília Berres4
1 Hospital de Clínicas de Passo Fundo, Neurocirurgia. Passo Fundo, Rio Grande do Sul, Brasil.
2 Hospital de Clínicas de Passo Fundo, Patologia. Passo Fundo, Rio Grande do Sul, Brasil.
3 Hospital de Clínicas de Passo Fundo, Residência em Neurocirurgia. Passo Fundo, Rio Grande do Sul, Brasil.
4 Faculdade Meridional IMED, Curso de Medicina. Passo Fundo, Rio Grande do Sul, Brasil.
Recebido em 26/05/2022
Aprovado em 24/10/2022
DOI: 10.21877/2448-3877.202200047
INTRODUCTION
Giant cell arteritis (GCA), also known as Horto disease or Temporal Arteritis, has an incidence that grows proportionately with aging, being the most frequent form of vasculitis in the elderly (incidence up to 200 cases / 100.000 people older than 60 years).(1) Nevertheless, it is extremely rare in the population younger than 50 years of age.(2,3) The incidence varies widely, according to gender, ethnics, and geographic region, being more common in women and in Asiatic patients and countries. It is a chronic, systemic disease, that usually affects the cranial vessels that originate from the aortic arch, but can compromise medium and large caliber vessels.(4)
The clinical scenario is wide, and the signs and symptoms are secondary to ischemia in the territory of the superficial temporal artery (STA) or any of its branches. The presence of the STA syndrome is highly suggestive of GCA, especially in patients older than 60 years.(5-8) In the present report, the authors describe one case of GCA with an atypical presentation.
CASE REPORT
We report the case of a 74-year-old female patient, with history of systemic arterial hypertension, diabetes mellitus and gastroesophageal reflux disease, who came to the emergency room (ER) complaining about progressive visual loss, headache and allodynia in the fronto-temporal region. The patient was struggling with a hemicranial intense headache for about 3 months, accompanied by photophobia and nausea, which were being treated as migraine. After starting treatment with Topiramate 50mg, the symptoms improved, but over weeks she developed recurrent episodes of visual loss, as well as periorbital and eye pain, predominantly with eye movement. After three days, the patient developed amaurosis in the right eye, and was evaluated by her ophthalmologist, who diagnosed unilateral papilledema, suggestive of optic neuritis. A couple of days later, the patient developed visual loss in the contralateral eye, being referenced to the ER.
In the ER, the patient complained of allodynia in the fronto-temporal region, associated with pain and swelling in the temporal artery topography (Figure 1). She was also complaining of pain in the temporo-mandibular articulation. Neurological examination evidenced bilateral papilledema, predominantly in her right eye, associated with decreased photopupillary reflex. An MRI was performed, which did not show any positive findings, as well as CSF analysis, although laboratory tests evidenced an elevation in the erythrocyte sedimentation rate, (> 100mm/hour).
Treatment with intravenous 1g of Methylprednisolone was administered for 3 days, but the patient did not show any improvement in her visual loss. After three days of treatment, the patient was submitted to STA biopsy, which confirmed the diagnosis of GCA (Figure 2). After discharge, the patient maintained treatment with Prednisone 60mg per day, but, to the date, she did not show any improvement in her visual deficit.
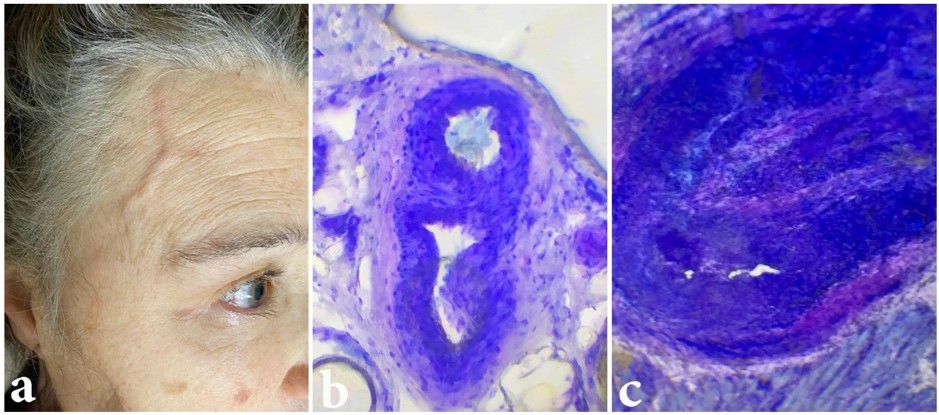
Figure 1
- a) Neurological examination evidencing swelling of the STA. b) Intra-operative analysis of the STA, evidencing normal segment of the biopsy sample. c) Intra-operative analysis of the STA, evidencing abnormal segment of the biopsy sample, with narrowing of the arterial light and inflammatory process.
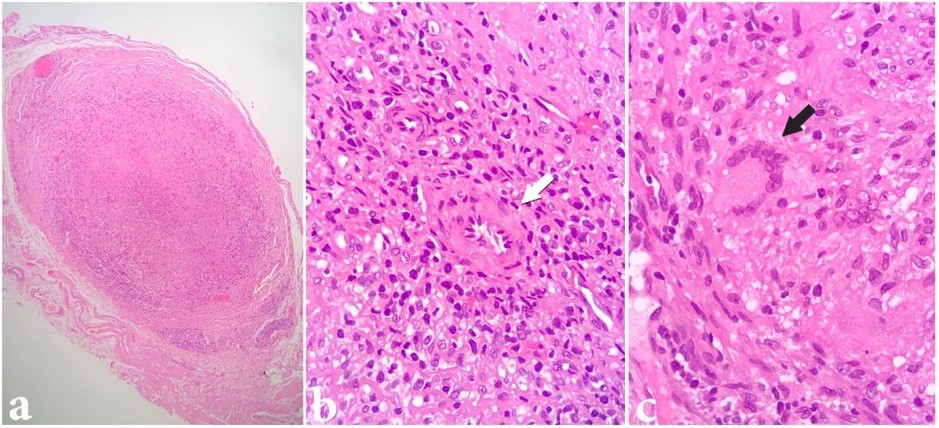
Figure 2
- a) H&E stain, 50x, evidencing intense inflammatory process in the artery wall, and a near total occlusion of the vessel. b) H&E stain, 200x, highlighting the narrowing of the artery light (white arrow). c) H&E stain, 200x, evidencing a granuloma with giant cells.
DISCUSSION
In general, patients with GCA present signs and symptoms secondary to ischemia in the vascular territory of STA. Among those, headache, tenderness in the scalp and jaw claudication are the most frequent and/or relevant. Temporal headache is the most common symptom, and jaw claudication the most specific for GCA, sometimes accompanied by trismus. The mandibular claudication occurs when there is involvement of the facial artery. The occurrence of acute, progressive, and severe visual loss is a characteristic signal of GCA, appearing mainly after the other symptoms, as described earlier. Classically, the visual loss is unilateral, but it can compromise the other eyeball after a period of days or weeks, and its occurrence depends on anterior ischemic optic neuropathy, due to the inflammatory thrombosis of the posterior branches of the ciliary arteries.(5-8)
The diagnosis is essentially made through the clinical scenario. A detailed evaluation of the clinical signs and symptoms and elevated clinical suspicion are essential. Laboratory findings are helpful, but they are unspecific, and cannot be trusted as a definitive tool for the diagnosis confirmation or exclusion.(9) Erythrocyte sedimentation rate (ESR) and reactive C-protein are usually high, but variation in both exams is wide and not specific.(9) This feature evidence the high value of outpatient follow-up. The American College of Rheumatology (ACR) is developing clinical criteria for diagnosis of GCA, although the sensibility of the scores is only about 75%.(4) More recently, a review made by the ACR enhanced the sensibility of the criteria to 93% and the specificity to 91,2%.(8) The criteria are: 50 or more years of age; recent onset and localized headache (occipital or frontal headache can be caused by temporal artery arteritis); temporal artery abnormalities; erythrocyte sedimentation rate (ESR) > 50 mm/hour; abnormal findings on temporal artery biopsy (containing necrotizing arteritis or multinucleated giant cells, for example).(1,10) If three or more criteria are present, the patient can be diagnosed with GCA.
Nevertheless, STA biopsy for histopathological evaluation remains the gold-standard for definitive diagnosis and should be performed in every patient.(7) There are two patterns of findings in the biopsy that define diagnosis: inflammation of the vessel walls (active arteritis – thickening of adventitia, media and intima, with preponderance of lymphocytes, macrophages and giant cells) and post-inflammatory abnormalities (healed arteritis – fibrosis of the vessel walls with disruption of the internal elastic lamina). The presence of multinucleated giant cells, which are a coalescence of macrophages, is very typical, but is not absolutely necessary in the biopsy.(7)
Treatment of GCA aims to prevent progression of the disease to visual loss, and, if present, to cause its remission. Immunosuppressive therapy with steroids is the mainstay of treatment. It can be performed through high-dose intravenous steroids, or through continuous administration of smaller doses, depending on the clinical scenario. The therapy must be initiated immediately after the clinical diagnosis and should not be delayed to after the biopsy of the STA is performed. The corticosteroid of choice is Prednisone, with starting dosage of 40 – 60mg orally in adults, increasing to as high as 100mg per day.(3) Unfortunately, even considering the collateral effects of prolonged steroid therapy, its efficacy is not that high. The progression of the disease is not rare, even in patients receiving optimized treatment. Special attention should be paid to the risk of amaurosis that, although not frequent, is very morbid, justifying the aggressive treatment.(11) In the present case, the disease progressed slowly, with symptoms lasting for 3 months, and the diagnosis was suggested after development of visual loss. The prognosis in those cases, opposite to the optic neuritis, is poor, and since amaurosis is established, the recovery of visual status rarely occurs.
CONCLUSION
GCA is a vasculitis that predominantly affects people older than 50 years and can result in severe visual loss or even amaurosis. It can also cause deterioration in other organs, since it is a systemic disease. Aggressive treatment is necessary to prevent decrease in visual status. There is still no definitive pathological etiology. In that way, it is very important that further research is performed, in order to understand the disease and to improve the therapeutic methods.
REFERENCES
- Pinheiro S, Horta A, Gomes P, Febra C, Ricardo A, Oliveira S, Góes MJ. Doença de Horton – a propósito de 40 casos. Revista da Sociedade Portuguesa de Medicina Interna. 2004, 11(1):7-12, março 2004. Disponível em: http://www.spmi.pt/revista/vol11/vol11_n1_2004_07_12.pdf. Acesso em: 03 Maio 2022.
- Godoy P, Araújo SA, Paulino-Júnior E, Lana-Peixoto MA. Arterite de Células Gigantes Coronariana e Infarto Agudo do Miocárdio. Arq Bras Cardiol. 2007, 88(4):84-87. Disponível em: http://www.scielo.br/pdf/abc/v88n4/27.pdf. Acesso em: 03 Maio 2022.
- Gonzalez EB, Varner WT, Lisse JR, Daniels JC, Hokanson JA. Giant-cell arteritis in the southern United States: an 11-year retrospective study from the Texas Gulf Coast. Arch Intern Med. 1989; 149: 1561-1565.
- Souza AW, Okamoto KY, Abrantes F, Schau B, Bacchiega AB, Shinjo SK. Giant cell arteritis: a multicenter observational study in Brazil. Clinics (São Paulo). 2013;68(3):317-22. doi: 10.6061/clinics/2013(03)oa06. PMID: 23644850; PMCID: PMC3611879.
- Hunder GG, Bloch DA, Michel BA, Stevens MB, Arend WP, Calabrese LH, Edworthy SM, Fauci AS, Leavitt RY, Lie JT, Lightfoot RW Jr, Masi AT, McShane DJ, Mills JA, Wallace SL, Zvaifler NJ: The American College of Rheumatology 1990 criteria for the classification of giant cell arteritis. Arthritis Rheum 33: 1122-1128, 1990
- Melges LDM, Novaretti TMS. Arterite de Células Gigantes, Marília. 1998. Disponível em: http://www.famema.br/ligas/ cefaleia/arterite.htm. Acesso em: 03 Maio 2022.
- Chacko, Joseph G et al. “Review of Giant cell arteritis.” Saudi journal of ophthalmology : official journal of the Saudi Ophthalmological Society 29,1 (2015):48-52. doi:10.1016/j.sjopt.2014.10.001
- Lana MA. Perda de visão e arterite de células gigantes. Soc Bras Retina e Vítreo. Conselho Brasileiro Oftalmologia. Belo Horizonte, 1998. Disponível em: http://www.cbo. com.br/cbo/sociedades/retina/artigos/cmtrato6.htm. Acesso em: 05 Maio 2022.
- Docken, MD. Diagnosis of giant cell arteritis. Post TW, ed. UpToDate. Waltham, MA: UpToDate Inc. https://www.uptodate.com. Acesso em: 14 set 2020.
- Almeida E. Diagnóstico e tratamento da arterite temporal. Disponível em: http://www.lincx.com.br/lincx/cientificos/ medicos/neurologia/arterite_temporal.asp. Acesso em: 05 Maio 2022.
- Bozza A, Levy R. Vasculites. Acta Médica Portuguesa, Maceió. 2003. Disponível em: http://www.lava.med.br/ livro/pdf/alda_vasculites.PDF. Acesso em: 05 Maio 2022.
Correspondência
Laura de Cezaro Martini
E-mail: [email protected]
