Papanicolau and Bethesda: a review on the evolution of classification in the cytological diagnosis of cervical-vaginal material
Papanicolau e Bethesda: uma revisão sobre a evolução da classificação no diagnóstico citológico do material cérvico-vaginal
João Lucas Silva de Luna1, Jayanne Clysse Oliveira de Souza2, José Queiroz Filho3, Janaína Cristiana de Oliveira Crispim4, Deyse de Souza Dantas5
1 Farmacêutico Oncológico – Universidade Federal do Rio Grande do Norte. Natal, RN, Brasil.
2 Farmacêutica – Universidade Federal do Rio Grande do Norte. Natal, RN, Brasil.
3 Doutor em Ciências da Saúde – Universidade Federal do Rio Grande do Norte. Natal, RN, Brasil.
4 PhD – Universidade Federal do Rio Grande do Norte. Natal, RN, Brasil.
5 Doutorado em Biologia Funcional e Molecular – Universidade Federal do Amapá/Universidade Federal do Rio Grande do Norte. Natal, RN, Brasil.
Recebido em 16/03/2021
Aprovado em 10/03/2022
DOI: 10.21877/2448-3877.202202125
INTRODUCTION
Cervico-vaginal cytology is a fundamental tool in screening for cervical cancer and its precursor lesions. Since the introduction of the cytological examination, several classifications have been proposed. Initially, the Papanicolau classification was proposed, described in Roman numerals from I to V, which classified the clinical findings according to the probability of being cancer or not. The Papanicolau classification separated lesions with the same potential for evolution to invasive carcinoma in different categories. From this limitation, the term dysplasia (graduated in mild, moderate and severe dysplasia) was included in 1953, by Reagan for lesions with lower oncogenic risk compared to carcinoma in situ.(1)
In 1969, a study was carried out by Richard and Barron demonstrating that untreated dysplasias had a high probability of progressing to carcinoma in situ, so they should not be classified in different degrees. Then, another classification was proposed to refer to the term dysplasia; the term CIN (cervical intraepithelial neoplasia) has been divided into three categories: CIN I (mild neoplasia), CIN II (moderate neoplasia) and CIN III (severe neoplasia or carcinoma in situ).(2)
With the various classifications for the release of cytopathological reports, there was no uniform standardization with regard to their release, each laboratory released in the way that best suited it, which generated a variability in the classifications used.
Due to this great variability in the findings of cervical cytology, there was an increasing need for standardization of these results, in order to solve what became known as “diagnostic chaos” in cytology. With that, in 1988, more precisely in December, in the Bethesda region, located in the US state of Maryland, a meeting with a multidisciplinary group of professionals specialized in the area of clinical cytology resulted in the creation of the Bethesda System or classification of Bethesda.(3) The evolution of the Pap smear classification to Bethesda is described in Table 1.
Table 1
Evolution of Papanicolau cytological nomenclatures in Bethesda.
| Papanicolau | Reagan | Richart | Bethesda System 1988 -1991 | Bethesda System 2001 – 2014 |
| Class I | Normal | Normal | Within normal limits | Negative for intraepithelial lesions or malignancy |
| Class II | Atypia | Atypia | ASCUS/AGUS | ASC-US/ASC-H |
| Class III | Mild dysplasia | NIC I | LSIL | LSIL |
| Class IV | Moderate, severe dysplasia or carcinoma in situ | NIC II ou NIC III | HSIL | HSIL |
| Class V | Invasive carcinoma | Invasive carcinoma | Invasive carcinoma | Invasive carcinoma |
The objective of the Bethesda System (TBS) was to establish a terminology that would provide clear limits for reducing variability among professionals, always in an attempt to improve the cyto-histological correlation. In the end it resulted in three principles that guide it until today. The first principle is that the terminology should communicate information that is clinically relevant to the health care of patients. The second principle is that the terminology should be uniform and reasonably reproducible by different pathologists and laboratories; present flexibility to be adapted to a wide variety of laboratories and geographic locations. The last, not least, principle is that the terminology needs to express the most current understanding of cervical neoplasia.(3)
According to these principles, even in 1988, TBS introduced a new terminology to report scaly intraepithelial lesions associated with the HPV cytopathic effect (SIL), divided into two categories, low and high grade, portraying different evolutionary potentials of these injuries. Low-grade cellular changes (LSIL) are lesions previously classified as NIC I. And high-grade cellular changes (HSIL) were previously classified as moderate dysplasia, severe dysplasia, carcinoma in situ, NIC II and NIC III. Thus, by classifying the lesions into only two LSIL and HSIL categories, it would result in less variability among observers, minimizing possible disagreement.(1) It is noteworthy that the classification of NIC is used until today in the field of pathological histology.
The TBS also included, in 1988, a term to standardize cytological changes that expressed doubts in cytologists and had indefinite characterization, insufficiently for a definitive interpretation. Resulting in the origin of the terms ASCUS (atypical squamous cells of undetermined meaning) and AGUS (atypical glandular cells of undetermined meaning). Therefore, for both categories of indeterminate cytological findings, a better clinical investigation is recommended, and should not be used as synonyms for terms such as atypia, benign atypia, inflammatory or reactive changes.(4)
In April 1991, three years after the initial publication of the Bethesda System, a second workshop was held to monitor and evaluate the use of this system in practice, with the aim of promoting improvements. To critically evaluate TBS, the workshop was attended by specialists from cytopathology and gynecology, who shared their clinical experiences in the practice of TBS. One of the main issues identified by the participants was the lack of uniform morphological criteria that designated specific terms of the TBS such as ASCUS. In 1994, the first Bethesda Atlas, also known as the “blue book”, was published, containing criteria, photographs and explanatory notes for all types of diagnosis, including ASCUS.(5)
A third meeting was held in 2001, for updates based on changes in practice and advances in science and technology. In this meeting, the exclusion of the term ASCUS was suggested by the minority of participants, who considered the nomenclature confusing. However, the elimination of ASCUS was not accepted, as it was considered essential since light microscopy has its limitations and it is not always possible to perform a definitive interpretation. In addition, the elimination of ASCUS could result in an increase in LSIL reporting and a decrease in HSIL, which did not contribute to cancer prevention.(6)
Instead, the term was differentiated into two categories: ASC-US (atypical squamous cells of undetermined significance) and ASC-H (atypical squamous cells that cannot exclude HSIL). The term AGUS was eliminated because the management of patients with glandular abnormalities has a great distinction, depending on the type of cell, in addition, the differentiation between endocervical and endometrial abnormalities must be recognized. Thus, the term ASC should be used in cases where the origin, both scaly and glandular, cannot be determined.(6)
That same year, they also had significant updates, such as the recommendation to use the terms “interpretation” or “result” instead of “diagnosis” for inclusion in the report of cervical cytology, because it is a screening test. The elimination of the “satisfactory, but limited by” statement for the Pap smear was, from then on, considered satisfactory or unsatisfactory for evaluation, and not classified as limited.(7)
TBS 2001 also suggested the removal of the expression “infection” and “reactive” which were secondarily called “organisms” and “other discoveries” respectively, in all cases that did not present epithelial abnormalities. In the same way that all negative results found in the Pap smear started to be reported under the interpretation of “negative for intraepithelial lesion or malignancy,” or “NILM”. TBS 2001, published the 2nd edition of the Bethesda atlas, with criteria for poor interpretation further information, explanatory notes and even new technologies such as liquid cytology, automation, computer-assisted imaging and tests for the detection of the HPV virus (human papilloma virus).(8)
The 2014 Bethesda System update brought few modifications to the terminology itself. Its most important change was regarding the notification of benign-looking endometrial cells, which is considered a normal finding during the woman’s proliferative phase, but which in postmenopausal women is considered abnormal, as it increases the sensitivity of a cancer of the endometrium. And after a literary review, the consensus was reached that it should be reported only in post-menopausal women or aged ≥ 45 years (when the information about the woman’s menstrual phase is unknown by the laboratory), instead of ≥ 40 years as indicated by the TBS in 2001.(8)
The main objective of this work was to analyze the evolution of cytological classifications of cervical-vaginal reports since the appearance of the Papanicolau classification to the Bethesda System, clarifying the evolution of the Bethesda system from the first edition of 1988 to the last edition, of 2014.
METHODS
This is a bibliographic review article on the evolution of Bethesda’s nomenclature in cervical vaginal material. The bibliographic survey of publications was carried out between February and May 2018. The online databases were used as a search tool: US National Library of Medicine (PubMed) and Scientific Electronic Library Online (SciELO), where scientific articles applicable to the proposed theme were selected.
For the search the following descriptors were used: “Bethesda” and “Terminology” and “Cytopathology” and “Cervical cytology”. The research took place in a broad way, in order to contemplate articles that reported on nomenclature in cervical vaginal cytology. Therefore, those who did not match the context of vaginal cervical cytology were excluded. Literature review articles were also excluded.
RESULTS
The research carried out resulted in a total of 185 scientific articles, collected by PubMed and SciELO. After analyzing the titles and abstracts, 27 articles were selected in PubMed and 8 articles in SciELO. Of the 185 articles found, 149 were excluded from the selection, as among several factors they dealt with related subjects, but which escaped the main focus of the work. The causes of exclusion are described below. (Figure 1)
The Bethesda System has gained wide acceptance by professionals in the field, and today this classification is the most used worldwide. Although it was developed mainly for cervical cytology, it served as a model for the development of other standardized notification systems in cytology and histopathology, such as the use of terminology in anogenital, vagina, thyroid samples, among others. The implementation of standardized terminology schemes facilitates the management of the cytopathologist to provide a more comprehensive report, in addition to reducing interobserver variability in the interpretation of results.
After reading in full, 14 articles were selected that met the inclusion criteria. And they are described in more detail in Table 2.
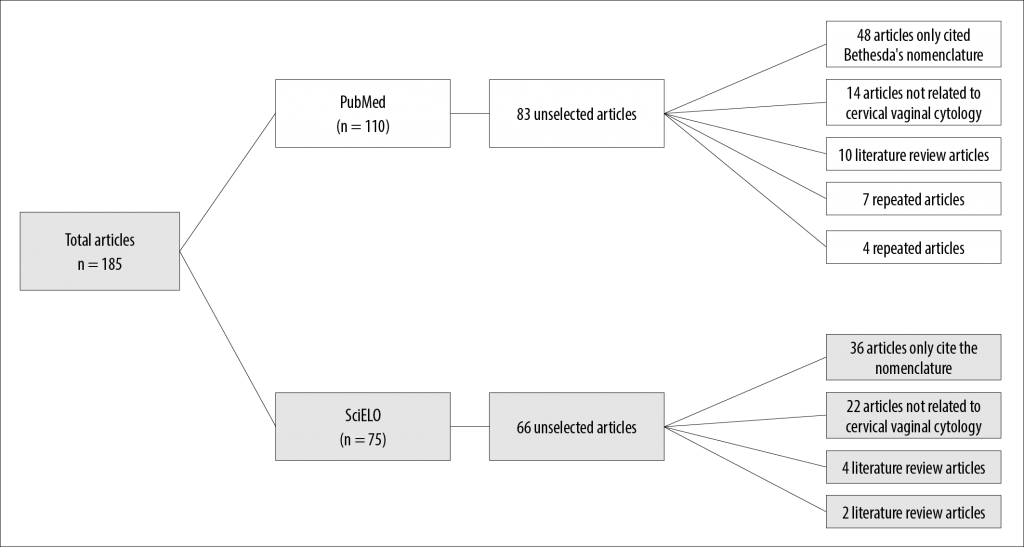
Figure 1
Flowchart of the articles found in the research according to the descriptors, and discarded after reading the title and abstract.
Table 2
Characterization of the articles included in this review.
| Title of the article | Authors | Study objectives | Main Results / Conclusions |
| The Bethesda 2001 system: updated terminology and application | Crothers(7) (2005) | Highlight the main updates of TBS 2001 and its application in clinical practice. | The majority of respondents (80.9% of 576) used a term that was not part of the Bethesda 2001 System to report low-grade squamous intraepithelial lesion, and cannot exclude a degree of squamous intraepithelial lesion (LSIL-H). |
| Bethesda’s system for reporting cervical cytology: a historical perspective | Nayar e Wilbur(5) (2017) | Clearly describe the Bethesda system from 1988 to 2014. | The success of TBS is based on solid principles that were instrumental in adopting and implementing it as a standardized notification terminology for cervical cytology. |
| Evaluation of Oncotic Colpocytology Blades Previously Diagnosed as ASCUS: Inter assay and interobserver comparison | Souza et al.(9) (2004) | To assess the existence of intra- and inter-cytopathological disagreement in the analysis of oncotic colpocytology slides that had previously been diagnosed with ASCUS and the degree of that disagreement. | Very distant degrees of agreement were observed between different analyzes by the same cytopathologist. Confirming the existence of subjectivity in ASCUS cytopathological reports. |
| Application fees and Bethesda 2001 reports | Davey et al.(8) (2004) | Analyze current laboratory reporting practices using Bethesda 2001 terminology and compare the results with data from previous 1996 research. | Of the 759 laboratories that answered the questionnaire, 85.5% had implemented Bethesda 2001 terminology, adopting important changes. New criteria and methods. |
| Effect of Bethesda 2001 on the ASC Report with Special Emphasis on Atypical Squamous Cells – Not Discarding High Grade (ASC-H) | Simsir et al.(10) (2005) | Compare the overall ASC rate and results for women with different categories of ASC before and after TBS 2001, to assess the impact of TBS 2001. | It has been confirmed that the consistent application of TBS 2001 for ASC reduces the ASC rate and better identifies women with high-risk injuries. |
| Impact of ASC-H terminology on HSIL detection in unattended Californian women | Howell et al.(11) (2008) | Determine whether this new terminology has made it easier to detect the most serious problems. | Thirteen percent of ASC-H showed CIN-III/CISThe introduction of the tern ASC-H was able to distinguish equivocal lesions that are more likely to represent serious injures, such as NICII/III/carcinoma in situ |
| The Papanicolau andd Bethesda 2014 | Nayar e Wilbur(3) (2015) | Highlight the main processes and the reason for the TBS update in 2014. | Pap test, still have useful around the world. Due to its greater specificity compared to the HPV test, which will be important as a diagnostic screening tool after a positive HPV test. |
| The Bethesda System 2001: an update of new terminologies for gynecological cytology | Henry(6) (2003) | Clarify Bethesda System updates 2001 | Explanations for the rapid acceptance of TBS are many, one of the main reasons is certainly the solid and thoughtful basis of all elements of TBS. |
| The impact of LSIL-H terminology on patient follow-up patterns: a comparison with LSHIL and ASC-H | Thrall et al.(12) (2013) | Study of a category not recognized by the Bethesda System, but which is commonly used, LSIL – H is a merger of the official LSIL and ASC-H categories | Although the clinical utility of the combined category is unclear, the research found a rate of discovery of high-grade dysplasia in biopsies higher for LSIL-H than LSIL and similar to ASC-H. |
| Impact of the More Restrictive Definition of Atypical Squamous Cells Introduced by the 2001 Bethesda System on the Sensitivity and Specificity of the Pap Test | Thrall et al.(13) (2008) | Evaluate the effect of eliminating ASCUS terminology – reactive factor and the sensitivity and specificity of this change in the Pap test. | By consensus of 4 observers, 32% of ASCUS cases were downgraded to NILM. The ASCUS threshold established by Bethesda 2001 prevents a considerable number of women from being monitored for ASC. |
| Notification fees from the Bethesda System for conventional Pap tests and liquid-based cytology tests in a large Chinese independent pathological medicine laboratory | Zheng et al.(14) (2015) | Document and analyze the reported rates of the Bethesda system for conventional Pap tests and liquid-based cytology between 2007 and 2012 at China’s largest College of American Pathologists. | Reported abnormality rates were significantly higher in liquid-based cytology than in conventional Pap smear. |
| ASC: SIL relationship after the implementation of the 2001 Bethesda System | Quddus et al.(15) (2004) | Compare the and the relationship between squamous intraepithelial lesions (ASC: SIL) before and after the implementation of TBS 2001, to see if there was an increase in ASC rates and ASC: SIL ratio. | Unsatisfactory sample rates and ASC remained unchanged. The 2001 TBS did not affect the ASC: SIL ratio or the abnormal detection rates of the Pap test. |
| The 2001 Bethesda System | Solomon et al.(16) (2002) | Report the history and main modifications of the Bethesda 20001 System. | The terminology of the 2001 Bethesda System reflects important advances in the biological understanding of cervical neoplasia. |
| Trends in cervical cytology screening and reporting practices | Crothers et al.(17) (2015) | Provide a cross-sectional study of gynecological cytology practices in 2010 through a questionnaire sent to participating laboratories at the College American of Pathologists. | After answering a questionnaire, 39% of the laboratories use a non-standard term of low-grade squamous intraepithelial lesion, not excluding squamous intraepithelial lesion, LSIL – H. |
DISCUSSION/CONCLUSION
The Bethesda System has gained wide acceptance by professionals in the field. Currently it is configured as being the most used classification worldwide. All of its evolution, from creation in 1988 to the last update in 2014, are described in Table 3. Although TBS was developed mainly for cervical cytology, it also served as a model for the development of other standardized notification systems in cytology and histopathology, such as the use of terminology in samples of the vagina, anus, thyroid, among others. The implementation of standardized terminology schemes facilitates the management of the cytopathologist to provide a more comprehensive and clear report, in addition to decreasing interobserver variability in the interpretation of results.(8)
Table 3
Main characteristics of the evolution of the Bethesda nomenclature from 1988 to 2014.
| TBS 1988 | TBS 1991 | TBS 2001 | TBS 2014 | |
| SAMPLE TYPE | Cervical or vaginal | Cervical or vaginal | Conventional smear, liquid foundation or other | Conventional smear, liquid foundation or other |
| SAMPLE SUITABILITY | Satisfactory for interpretation
Less than great Unsatisfactory |
Satisfactory for evaluation
Satisfactory for evaluation limited by (specify reason) Unsatisfactory for evaluation (specify reason) |
Satisfactory for evaluation (describe the presence of the endocervical / ZT component, blood, inflammation)
Unsatisfactory for evaluation (specify reason) |
Satisfactory for evaluation (describe the presence of the endocervical / ZT component, blood, inflammation)
Unsatisfactory for evaluation (specify reason) |
| GENERAL CATEGORIZATION (optional) | Within normal limits
Others: see descriptive diagnosis; recommended additional action |
Within normal limits
Benign cellular changes Abnormality of epithelial cells |
Negative for intraepithelial injury or malignancy
Others: It is recommended to see endometrial cell results in women ≥ 40 years old Abnormal epithelial cells (specify whether in squamous or glandular cells) |
Negative for intraepithelial injury or malignancy
Others: It is recommended to see endometrial cell results in women ≥ 45 years old |
| DESCRIPTIVE DIAGNOSIS
(1988 – 1991) INTERPRETATION / RESULT (2001 – 2014) |
DESCRIPTIVE DIAGNOSIS
IINFECTION Fungi, bacteria, protozoa, viruses, other (Note: if HPV refers to epithelial squamous cell abnormalities) REACTIVE AND REPARATIVE CHANGES Inflamation: – Associated with cellular changes, follicular cervicitis. – Miscellaneous (patient history) – Effects of therapy, radiation, chemotherapy, IUD, Others Abnormalities of epithelial cells SQUAMOUS CELLS Atypical squamous cells of undertemined significance (ASC-US) (follow-up or further investigation recommended) Squamous intraepithelial lesion (SIL) Low-grade scaly lesion (LSIL) Covering: changes associated with HPV /mild dysplasia /CIN I High-grade scaly lesion (HSIL) Covering: moderate dysplasia CIN II / severe CIN III / carcinoma in situ CIN III Squamous cell carcinoma GLANDULAR CELLS Report the presence of endometrial cells in the following circumstances: woman is not menstruating, post menopause, no history of menstruation Atypical gland cells of undetermined significance (AGUS) Endometrial, endocervical, unspecified Adenocarcinoma Specify probable place of origin: endocervical, endometrial, extrauterine Not specified NON-EPITHELIAL MALIGNA NEOPLASIA (to specify) HORMONAL EVALUATION (applied to vaginal smears only) – Hormonal pattern compatible with age and history – Hormonal pattern incompatible with age and history (specify) – Hormonal evaluation is not possible: Cervical sample, inflammation, insufficient patient history
|
DESCRIPTIVE DIAGNOSIS
BENIGN CELL CHANGES Infection: – T. Vaginalis – Fungal organisms morphologically consistent with Cândida spp. – Cellular changes with Herpes simplex vírus Reactive changes Reactive cellular changes associated with: Inflammation, atrophy with inflammation, radiation, IUD, others. Epithelial cell abnormalities
SQUAMOUS CELLS Atypical epithelial cells of undetermined significance (ASC-US) Low-grade squamous intraepithelial lesion (LSIL) Covering: HPV / mild dysplasia / CIN I High-grade squamous intraepithelial lesion (HSIL) Covering: Moderate dysplasia / severe dysplasia and carcinoma in situ / CIN II AND CIN III Squamous cell carcinoma GLANDULAR CELLS Endometrial cells, benign cytology, postmenopausal women Atypical gland cells of undetermined significance (AGUS): Qualify: Adenocarcinomaendocervical, endometrial adenocarcinoma, extrauterine adenocarcinoma, unspecified adenocarcinoma. |
INTERPRETATION / RESULT
Negative for intraepithelial injury or malignancy (NILM) ORGANISMS: – T. Vaginalis – Fungal organisms morphologically consistent with Cândida spp. – Flora change suggestive of bacterial vaginosis – Bacterium morphologically consistent with Actinomyces spp. – Cellular changes associated with Herpes simplex vírus NON-NEOPLASTIC FINDINGS (OPTIONAL) Reactive cell changes associated with: – Inflammation, radiation, IUD Others Endometrial cells (in women ≥ 40 years old) (specify if negative for intraepithelial lesion) Abnormalities in epithelial cells SQUAMOUS CELLS Atypical squamous cells – Undetermined meaning (ASCUS) – Does not exclude HSIL (ASC-H) Low-grade intraepithelial lesion: HPV / mild dysplasia / CIN I High-grade intraepithelial lesion: moderate dysplasia and severe dysplasia, CIN II and CIN III) – Squamous cell carcinoma GLANDULAR CELLS Atypical -Endocervical, endometrial cells, gland cells -Endocervical cells favor neoplasia -Endometrial cells favor neoplasia, endocervical adenocarcinoma in situ Adenocarcinoma -Endocervical, endometrial, extrauterine, unspecified OTHER MALIGNANT NEOPLASMS (to specify) |
INTERPRETATION / RESULT
Negative for intraepithelial injury or malignancy (NILM) ORGANISMS: – T. Vaginalis – Fungal organisms morphologically consistent with Cândida spp. – Flora change suggestive of bacterial vaginosis – Bacterium morphologically consistent with Actinomyces spp. – Cellular changes associated with Herpes simplex vírus NON-NEOPLASTIC FINDINGS (OPTIONAL – Inflammation – Radiation – IUD – Gland cells in women with hysterectomy
Abnormalities in epithelial cells SQUAMOUS CELLS – Squamous cell of undetermined significance (ASC-US) – Squamous cell of undetermined significance not excluding high-grade injury (ASC-H) – Low-grade intraepithelial lesion (LSIL): HPV / mild dysplasia / CIN l High-grade intraepithelial lesion (HSIL): moderate dysplasia and severe dysplasia, CIN II and CIN III) – Squamous cell carcinoma GLANDULAR CELLS – Endocervical cell favors neoplasia – Endometrial cell favors neoplasia Adenocarcinoma endocervical in situ Adenocarcinoma – Endocervical, endometrial, extrauterine, unspecified OTHER MALIGNANT NEOPLASMS (to specify) |
| OTHERS | ||||
| AUXILIARY TESTS (if appropriate) | If it is useful to recommend additional tests that can complement cytology. | If it is useful to recommend additional tests that can complement cytology. | ||
| AUTOMATED EVALUATION (revise if appropriate) | If the assessment is automated, specify which equipment is used and the result. | If the assessment is automated, specify which equipment is used and the result. | ||
| EDUCATIONAL NOTES AND SUGGESTIONS (optional) | Concise, but not directive, suggestions, according to the clinical follow-up guidelines, and formulated in the form of a suggestion. | Concise, but not directive, suggestions, according to the clinical follow-up guidelines, and formulated in the form of a suggestion. | ||
The TBS, when creating a standardized report, includes an evaluation for sample adequacy in “satisfactory”, “satisfactory, but limited by” and “unsatisfactory”, being the most important component of the sample’s quality assurance. However, in 2001 the category “satisfactory, but limited by” was eliminated, because the term was considered confusing for many doctors and therefore several tests were performed repeatedly without need. In a survey of 760 laboratories by Davey et al.(8) it was shown that more than 85% of the laboratories eliminated the “satisfactory, but limited by” category. In the same year Quddus et al.(15) stated that the elimination of this category had not increased the number of cases, classified as “unsatisfactory” as they suspected it could happen.
TBS 2001 recommended the use of the term “interpretation” or “result” to be described in the report, rather than “diagnosis” as previously reported. Crothers et al.(7) say that the Papanicolau test reflects only the cytological criteria of the lesions and that there is an inherent subjectivity of the evaluation. Thus, the test should serve as a screening and not a diagnosis. For the “infection” category, the use of the term “organisms” was recommended, because not all organisms cause infection, but it can represent colonization.(6)
The ASC diagnostic category was the most controversial interpretation term since its introduction in TBS in 1988, due to limitations in morphological interpretation due to lack of criteria. The vast majority of the results found in cytology were in the ASCUS / LSIL category, leading a large number of women to colposcopy, which represented a clinical problem Nayar and Wilbur.(5) During the TBS 2001 update, it was suggested to exclude this term, but this did not occur, so that there was no loss of sensitivity for a positive HSIL that could be pronounced. For Henry(6) the elimination of ASC could result in an increase in LSIL reports and a decrease in HSIL.
The ASC category was therefore maintained, but with some changes and with more restricted definitions, classified in ASC-US and ASC-H only. The ASC-R (favor reactive) category was commonly used, and the ASC-US category was combined in the TBS 2001. In a study by Simsir(10) after the implementation of the TBS 2001, it showed that the percentage of women with low and high grade was no different before and after TBS 2001, and ASC-R had a very small risk for NIC II / III similar to ASC-US confirming that ASC subclassification had no effective clinical significance. In that same study it was seen that the ASC rate decreased after the implementation of TBS 2001, and ASC-H identified more high-grade injuries and less than low-grade injuries. The percentage of women receiving ASC-H colposcopy increased by 70% before and 81% after the update. There was no significant difference for ASC-US.
Howell(11) corroborates the results found by Simsir(10), and says that the introduction of the term ASC-H seems to have achieved its purpose of identifying more serious injuries such as CIN II / III / CIS (carcinoma in situ), once that suspected HSIL has important implications and different follow-up strategies, for an ASC-H result is recommended by ASCCP (College of American Pathologists), colposcopy and biopsy immediately. Today, for ASC-US results, the HPV screening test is increasingly performed, which reduced the referrals for colposcopy by 50% according to Nayar and Wilbur.(5)
The Bethesda System since its creation in 1988, divides squamous intraepithelial lesions into LSIL and HSIL, as a way to reduce the variability of interpretation between observers. However, in a study by Crothers et al.(17) with 625 laboratories, 80.9% of these confirmed to use a term that is not part of the Bethesda System, a low-grade squamous intraepithelial lesion, does not exclude a degree of squamous intraepithelial lesion (LSIL-H) for tests where obvious cells of LSIL are seen, but it also contains cells that may represent HSIL. And it affirms the need for a terminology that identifies this situation.
Trhall et al.(12) stated the use of the same term (LSIL-H) and compared it to the results of ASC-H, according to the authors, the rate of high-grade dysplasia in LSIL-H biopsies (31.9%) was similar to ASC- H (35.3%) and greater than LSIL (7.6%) and recommends that it be treated clinically in a similar way to ASC-H. However, the use of this non-standard term can lead to confusion in clinical management and go against the principles of the Bethesda System.
Communication through a universal language is of great value for the health area, because it is thus possible to compare experiences and clinical data, which is exactly what the Bethesda System did – a terminology that could be understood by different observers anywhere in the world. world; contributing to decrease the variability of diagnoses, thus positively impacting patient care. One of the most significant contributions of TBS was that it served as a model for the development of other standardized reporting systems, both in cytopathology and in histopathology.
It is also natural that they can be modified as science and technology evolve, leading to the need for continuous TBS updates. With the implementation of HPV prophylactic vaccination programs for cervical prevention, the number of smears will decrease and could be even more challenging.
STATEMENTS
Statement of ethics
The following systematic review does not need to go through an ethics committee.
AUTHOR CONTRIBUTIONS
Each author participated sufficiently in this submission to take public responsibility for the content and have approved publication.
REFERENCES
- Consolaro MEL; Engler SSM. Citologia clínica cérvico vaginal: texto e atlas. Grupo Gen-Editora Roca Ltda., 2000.
- Richart RM; Barro BA. A follow-up study of patients with cervical dysplasia. American journal of obstetrics and gynecology.1969;105(3):386-393.
- Nayar R; Wilbur DC. The Pap Test and Bethesda 2014. Acta Cytologica. DOI:10.1159/000381842.
- Sebastião APM, Noronha L, Scheffel DLH, Garcia MJ, Carvalho NS, Collaço LM et al. Estudo das atipias indeterminadas em relação à prevalência e ao percentual de discordância nos casos do Programa de Prevenção do Câncer Uterino do Paraná. J. Bras. Patol. Med. Lab. DOI:10.1590/S1676-24442004000600012.
- Nayar R; Wilbur DC. The Bethesda system for reporting cervical cytology: A Historical perspective. Acta cytologica. 2017;61(4-5):359-372.
- Henry MR. The Bethesda System 2001: an update of new terminology for gynecologic cytology. Clinics in laboratory medicine. 2003;23(3):585-603.
- Crothers BA. The Bethesda System 2001: update on terminology and application. Clinical obstetrics and gynecology. 2005;48(1):98-107.
- Davey DD. et al. Bethesda 2001 implementation and reporting rates: 2003 practices of participants in the College of American Pathologists Interlaboratory Comparison Program in Cervicovaginal Cytology. Archives of pathology & laboratory medicine. 2004;128(11): 1224-1229.
- Souza JHK de et al. Avaliação de lâminas de colpocitologia oncótica previamente diagnosticadas como ASCUS: comparação interensaio e interobservadores. Rev Bras Ginecol Obstet. 2004;26(3): 233-240.
- Simsir A et al. Effect of Bethesda 2001 on reporting of atypical squamous cells (ASC) with special emphasis on atypical squamous cells‐cannot rule out high grade (ASC‐H). Diagnostic cytopathology. 2006;34(1):62-66.
- Howell LP; Gurusinghe S; Tabnak F. Impact of ASC‐H terminology on the detection of HSILs in medically underserved California women. Diagnostic cytopathology. 2009;37(2):103-110.
- Thrall MJ; Galfione SK; Smith DA. The impact of LSIL‐H terminology on patient follow‐up patterns. Diagnostic cytopathology. 2013;41(11):960-964.
- Thrall MJ et al. Impact of the more restrictive definition of atypical squamous cells introduced by the 2001 Bethesda System on the sensitivity and specificity of the Papanicolaou test. Cancer Cytopathology. 2008;114(3):171-179.
- Zheng B et al. Bethesda system reporting rates for conventional Papanicolaou tests and liquid-based cytology in a large Chinese, College of American Pathologists certified independent medical laboratory: analysis of 1 394 389 Papanicolaou test reports. Archives of Pathology and Laboratory Medicine. 2015;139(3):373-377.
- Quddus MR et al. ASC: SIL ratio following implementation of the 2001 Bethesda System. Diagnostic cytopathology. 2004;30(4):240-242.
- Solomon D et al. The 2001 Bethesda System: terminology for reporting results of cervical cytology. Jama. 2002;287(16):2114-2119.
- Crothers BA et al. Trends in cervical cytology screening and reporting practices: results from the College of American Pathologists 2011 PAP education supplemental questionnaire. Archives of pathology & laboratory medicine. 2015;140(1):13-21.
Correspondência
João Lucas Silva de Luna
E-mail: [email protected]
